Greetings, and thank you for turning to another edition of the Gist Weekly! Please feel free to forward this email to friends and colleagues, and encourage them to subscribe as well.
In the News
What happened in healthcare recently—and what we think about it.
- Hims & Hers unveils $199 weight-loss shots. On Monday, telehealth company Hims & Hers announced it will offer a compounded version of the GLP-1 drug semaglutide starting at $199 per month, which is 85 percent off the list price of Wegovy, Novo Nordisk’s branded semaglutide drug. Hims & Hers’ compounded version of the injectable weight-loss medication will be prescribed by a physician through its own telehealth platform. Compounded drugs bypass the Food and Drug Administration (FDA)’s standard approval process, but Hims & Hers CEO Andrew Dudum stated that its compounded semaglutide will be made in a FDA-licensed facility that is one of the largest manufacturers of generic medications in the country.
- The Gist: Brand-name weight-loss drug manufacturers are facing scrutiny for their high drug prices and have been unable to keep up with demand. As long as semaglutide remains in shortage, the FDA allows compounding pharmacies to make copycat versions of the drug without violating patent laws. Although some consumers may be deterred by the compounded drugs’ lack of FDA oversight, given that about half of US adults say they would be interested in taking a safe and effective prescription weight-loss drug, Hims & Hers’ new offering could potentially transform the access landscape for these treatments.
- CMS launches an emergency care complaint portal. On Tuesday, the Centers for Medicare and Medicaid Services (CMS) announced an overhaul to the complaint filing process for patients who feel they’ve been denied care in violation of the Emergency Medical Treatment and Labor Act (EMTALA). The federal law requires hospitals, on condition of receiving federal funds, to stabilize or transfer patients who need emergency care without discrimination. Although CMS is tasked with enforcing the law, state agencies were responsible for collecting complaints in the previous reporting process, which was criticized for being overly complex and varying too much by state. Now, patients can access a portal to file complaints directly with CMS, a change that’s intended to expedite the federal government’s ability to investigate potential EMTALA violations as well as improve enforceability of the law and transparency into emergency care access.
- The Gist: The wave of state-level abortion bans passed after the Supreme Court’s 2022 decision to overturn Roe v. Wade has made EMTALA enforcement a highly politicized issue. Many physicians and hospital leaders in these states have expressed confusion concerning the legality of emergency abortions. This conflict between state and federal laws is expected to be ruled on later this summer by the Supreme Court, which recently heard arguments on whether EMTALA takes precedence over Idaho’s highly restrictive abortion ban. Although abortion restrictions have raised EMTALA’s profile, the new, consumer-friendly portal should help protect the rights of patients seeking any type of emergency service, replacing a process that many patients have struggled to navigate.
- Senate Finance Committee signals interest in Medicare physician payment reforms. Last Friday, the US Senate Finance Committee released a white paper outlining potential reforms to Medicare’s physician fee schedule, framing it as “the foundation for another impactful legislative effort.” In the paper, the committee expressed interest in tying annual conversion factor updates to the Medicare Economic Index (MEI) to account for practice cost inflation in a more predictable way. The committee also said it’s exploring Medicare’s budget neutrality provision, which legally requires CMS to balance payment increases in some physician specialties with decreases other specialties if relative value unit (RVU) changes will increase its annual spending by more than $20M. Provider groups like the Medical Group Management Association (MGMA) are “encouraged” by the white paper, but no corresponding legislation has been thus far introduced.
- The Gist: Meaningful legislative action addressing practice cost inflation and loosening budget neutrality requirements would go a long waytoward stabilizing the long-term health of many physician practices. Unlike Medicare payments to hospitals, Medicare physician reimbursement has significantly lagged both the MEI and consumer price index since 2001. Although the Finance Committee’s interest in Medicare physician payment should give providers some hope of future relief, theimmediate legislative prospects for these policies appear slim during an election year, and there’s no guarantee that these issues will remain on the table in a new Congress.
Plus—what we’ve been reading.
- Comparing the cost-effectiveness of two weight-loss treatments. Published last month in JAMA, this study analyzes the cost-effectiveness of two different weight-loss treatments: endoscopic sleeve gastroplasty (ESG), a minimally invasive procedure, and semaglutide, an injectable GLP-1 drug. The study compared the cost of each treatment along with the quality-adjusted life-years (QALYs) gained over a five-year span from treating class II obesity with each measured against a baseline no-treatment strategy. Accounting for mitigating factors such as patient drop-out risk in the semaglutide group and adverse events in the ESG group, the study found that patients who underwent ESG sustained more weight loss, with their average body mass index (BMI) dropping from 37.0 to 31.7 after five years, compared with dropping to 33.0 for semaglutide users. ESG was also associated with lower costs after two years. Given these results, the authors suggest that treatments like ESG could potentially help ease the potential budget strain expected from the increasing use of semaglutide.
- The Gist: Although this study looked at semaglutide’s effect on weight loss alone, and not on its benefit associated with improvement in comorbidities, the drug has also been approved for type 2 diabetes as well as reducing the risk of cardiovascular disease, which changes its cost-effectiveness calculus for many patients. Patients seeking weight-loss treatments also havedifferent personal preferences, levels of risk toleration, and cost considerations than just the overall cost-effectiveness of a specific treatment to the healthcare system. Additionally, whether from compound pharmacies or the government, increasing competition may end up driving down the price of branded semaglutide drugs.
Graphic of the Week
A key insight or teaching point from our work with clients, illustrated in infographic form.
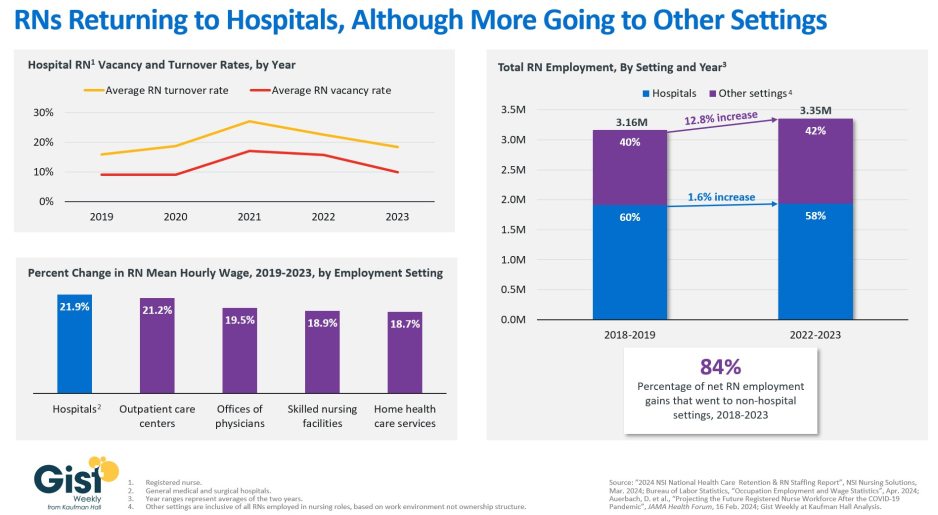
Hospital nursing shortage appears to be abating
In this week’s graphic, we analyze the state of the nursing workforce four years after the acute staffing shortages induced by the pandemic began. The nursing labor crisis has largely subsided at most hospitals. After peaking in 2021, the average hospital’s registered nurse (RN) turnover and vacancy rates in 2023 have nearly returned to 2019 levels, at 18 percent and 10 percent respectively. Provider organizations of all types have attracted nursing talent through wage increases. Hospital-employed RNs saw a nearly 22 percent pay increase between 2019 and 2023, setting a higher floor for hospital labor costs. Although there were more employed RNs in hospital settings in 2023 than there were in 2019, 84-percent of net RN employment gains over that time period have been to non-hospital settings. This increase is likely a result of the pandemic accelerating the ongoing outpatient shift. While some individual hospitals and certain regions of the country may still be experiencing RN shortages, many organizations are now shifting their focus to longer-term labor strategy rather than short-term staffing challenges.
On the Road
What we learned from our work in the real world. This week from Brian Pisarsky, Managing Director, at Kaufman Hall.
Engaging hospitalists in reducing length of stay
A health system CEO I’ve worked with over the years called me up recently to revisit a familiar topic. “Our average length of stay has plateaued again. We were making good progress ratcheting it down from pandemic highs, but it’s been stuck at about 5.5 days for the better part of a year, which we can’t afford right now. What else can we try to reduce it?”
Lowering length of stay is definitely a no-regrets strategy, especially today, for its myriad benefits, including lowered operating costs, improved revenue from additional admissions, and avoided capital spend for new buildings or patient bed towers. But of course, reducing it is an organization-wide challenge with many moving parts. One trend I’ve been seeing in hospitals with at or below average expected length of stay is how their hospitalists are fully engaged and aligned with their care transitions and nursing teams in patient throughput efforts. Hospitalists can be involved from the very beginning of a patient’s stay, working with emergency department physicians to ensure that correct patient status is captured from the start. Hospitalists should also be involved in daily discharge planning conversations during multidisciplinary rounds. Their expertise is vital in making quicker decisions about patients throughout their stay, as well as in peer-to-peer physician exchanges with patients’ insurers on issues like post-acute placement. If your health system is interested in better engaging hospitalists in patient throughput and length of stay improvement efforts, I’m happy to share more. Please don’t hesitate to reach out.
On Our Podcast
Gist Healthcare Daily—all the headlines in healthcare policy, business, and more, in ten minutes or less every weekday morning.
In addition to the news discussed above, our Gist Healthcare Daily podcast covered many of the week’s other big stories, including the DOJ moves to classify marijuana as a less dangerous drug, the latest 340B ruling is a win for drugmakers, and the Senate Judiciary Committee scrutinizes the patent system’s role in high prescription drug prices.
To stay up to date, be sure to tune in each weekday morning. Subscribe on Apple, Spotify, Google, or wherever fine podcasts are available.
Thanks for joining us, and we wish you a relaxing Memorial Day weekend. We’ll be back with more next Friday but, in the meantime, please visit our archive if you’d like to peruse past editions of the Gist Weekly.
Best regards,
The Gist Weekly team at Kaufman Hall




