Hello, and welcome back to this week’s edition of the Gist Weekly. Before we start with this week’s news, the enactment of the One Big Beautiful Bill (OBBB) has clearly been a prominent story this week. Given the immense potential impacts on providers and patients, our team continues to monitor how this legislation will affect the healthcare industry and looks forward to providing further analysis in the coming weeks. As always, we appreciate your continued readership and invite you to forward this email to friends and colleagues—please encourage them to subscribe!
In the News
What happened in healthcare recently—and what we think about it.
- More insurers feeling cost pressures. Molina Healthcare announced its preliminary second quarter financial results and adjusted its earnings guidance on Monday. The managed care company reported that its net income declined 14% during the second quarter and lowered its expected profits per share from a minimum of $24.50 to between $21.50 and $22.50. Joseph Zubretsky, Molina’s president and chief executive officer, said “the short-term earnings pressure we are experiencing results from what we believe to be a temporary dislocation between premium rates and medical cost trend, which has recently accelerated…nothing, including the potential impacts of the budget bill, has changed our outlook for the long-term performance of the business.” The news comes just a week after its competitor Centene withdrew its earnings guidance after over-projecting its exchange plan risk-adjustment payments.
- The Gist: If UnitedHealth Group’s financial challenges earlier this year weren’t enough of a sign, the golden age for payers appears to be over. Notably, payers are struggling before they truly feel the effects of OBBB on Medicaid and the potential sunsetting of enhanced subsidies on the exchanges—actions that will likely lead to significant coverage losses in Molina’s and Centene’s core markets. The drive to “repeal and replace” the Affordable Care Act (ACA) has subsided, but scrutiny and new regulations are weakening the ACA-enabled exchanges. While most states have not yet reported, average marketplace premiums could rise 17.4% next year, an increase that could lead to more adverse selection and greater financial challenges for these payers.
- Supreme Court ruling allows federal layoffs to continue. On Tuesday, the Supreme Court lifted a district court ruling blocking the layoffs of federal workers at almost two dozen agencies. This order will allow the Trump administration to continue reorganizing and cutting back the size of the federal bureaucracy, which the president has long criticized. This reduction-in-force (RIF) affected the Department of Health and Human Services (HHS), with a late March announcement stating that HHS would downsize from 82,000 to 62,000 full-time employees, combining layoffs with early retirements.
- The Gist: With just one dissenting opinion from Justice Ketanji Brown Jackson, there appears to be widespread consensus among the justices that the executive actions initiating the RIFs were lawful. This decision did not, however, condone the legality of specific layoffs. This leaves the door open for continued legal action. In a concurring opinion, Justice Sonia Sotomayor stated, “the President cannot restructure federal agencies in a manner inconsistent with congressional mandates… the plans themselves are not before this Court.” The current state of the layoffs heavily affected critical work at HHS, disrupting research, disease monitoring and more. It looks like this won’t be resolved anytime soon.
- U.S. measles cases at highest level since 1992. The United States is now at the highest yearly total of measles cases since 1992. The Centers for Disease Control and Prevention (CDC) reported on Wednesday that as of July 8, 1,288 cases have been confirmed in the United States in 2025. Of these, 92% occurred in patients who were unvaccinated or had an unknown vaccination status. There have been 27 measles outbreaks so far this year, with 88% of the confirmed cases associated with an outbreak. Measles was declared eliminated in the United States in 2000.
- The Gist: This is a grim milestone to reach at the midpoint of the year. Should measles spread endemically for 12 months, the United States could lose its measles elimination status, which appears more likely by the day. The increasing return of measles brings a unique challenge to clinical providers, who may have to reacquaint themselves with treatment and diagnosis protocols. Despite the effectiveness of childhood vaccines, vaccination coverage is falling, exemption rates vary widely by state and trust in public health officials is declining. HHS Secretary Robert F. Kennedy Jr.’s controversial statements and actions as Secretary on vaccines also muddy the waters for patients seeking clarity. Should childhood vaccination rates continue to decline, the consequences could be dire.
Plus—what we’ve been reading.
- The power of a patient’s story. Published in early June in Health Affairs, this narrative from David Dranove, an economist and professor of health industry management, chronicles his bladder cancer journey. Dranove considers how difficult it is to be a good healthcare consumer. In excerpts from across a year’s journal entries, Dranove’s journey highlights the high-stakes decisions he made in navigating the healthcare delivery system: from early self-misdiagnosis to provider selection and referrals, to relying on his care team for support in lieu of available data and communicating with insurers about the financial impact of his care. He reflects on his journey, sharing insights and advocating for more accessible quality reporting for patients and cost transparency from insurers.
- The Gist: Even for health policy experts, navigating healthcare is difficult, and being a “good consumer” is a tall order. Public data needed to make smart consumer decisions remains difficult to find, even for healthcare insiders who know what to look for. Quality metrics and cost transparency information also are limited in providing actionable insights for patients who need to make consequential provider and care selection decisions and understand the full financial and clinical impact of their decisions. While this year’s price transparency executive order aims to help provide patients with actionable information, implementation and compliance have a long way to go.
Graphic of the Week
A key insight illustrated in infographic form.
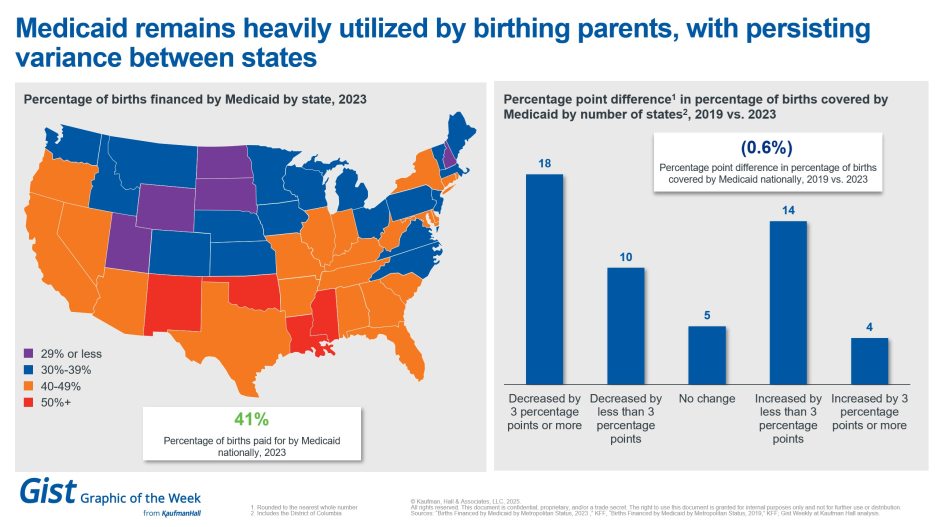
Medicaid a prominent coverage provider among birthing parents
In light of Medicaid cuts in the now-signed OBBB becoming law, this week’s graphic highlights a prominent use of Medicaid. Even though only about 1 in 5 people are covered by Medicaid, in 2023, more than 4 in 10 births in the United States were covered by Medicaid. There is significant variation among states; nearly two-thirds of births in Louisiana were covered by Medicaid while only 21% of births in New Hampshire were. Notably, only Utah was below the national Medicaid coverage rate at 18% of births. While the national Medicaid birthrate has been steady since 2019, there has been measurable change on a state-by-state basis. Eighteen states saw a 3-percentage point decrease in the Medicaid birth rate over this time while 4 saw the opposite. Only 5 saw no change between 2019 and 2023. While increasing the birth rate remains a priority for President Trump, a changing coverage environment could become a new factor for some couples to weigh.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
As health systems have prioritized their core operating platforms, real estate – especially non-acute real estate like medical office buildings (MOBs) – has often been treated as a cost center needed to support the delivery of care.
In a new article, Robert Turner and William Earl discuss the “real estate blind spot” around assets like MOBs. When these assets are actively managed for financial performance instead of sitting idle on the balance sheet as a depreciated asset, they can play an important role in liquidity enhancement, credit positioning and total capital efficiency.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business, and more, in ten minutes or less every other weekday morning.
On Monday, Gist Healthcare Podcast host J. Carlisle Larsen is joined by Modern Healthcare's Michael McAuliff to talk more about the passage of the One Big Beautiful Bill Act.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever fine podcasts are available.
Thanks for reading! We’ll see you next Friday with a new edition. In the meantime, check out our Gist Weekly archive if you’d like to peruse past editions. We also have all of our recent “Graphics of the Week” available here.
Best regards,
The Gist Weekly team at Kaufman Hall








