In the News
The biggest news of the week—and what we think about it.
- Strongest job growth in a year fueled by healthcare. Healthcare remains the engine of the U.S. economy, as the nation’s new jobs report indicates that more than half of all jobs added in January came from the field. According to the report, released this week by the U.S. Bureau of Labor Statistics, 82,000 of the 130,000 new jobs created last month were in healthcare. The unemployment rate edged down to 4.3% in December and wages increased. Gains included 50,000 jobs in ambulatory health services, 18,000 in hospitals and 13,000 in nursing and residential care facilities. Employment in social assistance also rose by 42,000, largely in individual and family services, which added 38,000 positions. Economists cautioned that the heavy reliance on healthcare hiring and job losses in other, higher-paying sectors temper enthusiasm about the economy.
- The Gist: Last year, job growth in healthcare averaged 33,000 per month. January’s report shows that momentum continues, with healthcare accounting for the bulk of the month’s gain. The demand for healthcare workers signals the field’s underlying strength. Even as some better-paying industries struggle, steady demand for healthcare has helped keep the job market steady. Experts say the trend will continue, as healthcare requires a skilled workforce to perform labor-intensive work as the population ages.
- ACO adoption continues to climb: CMS. Enrollment in Medicare accountable care organizations (ACO) continues to climb, according to figures released last week by the Centers for Medicare & Medicaid Services (CMS). CMS reported that as of last month, an estimated 14.3 million Medicare beneficiaries were aligned with an ACO, up about 4.4% from last year, reflecting growth in the Medicare Shared Savings Program (MSSP) and models like ACO REACH. CMS approved 134 new or returning MSSP applications for 2026, bringing total participation to 511 ACOs and more than 700,000 providers and organizations serving traditional Medicare beneficiaries. Other specialized models such as Kidney Care Choices and the PC Flex Model also expanded their reach. Additionally, CMS unveiled the Long-term Enhanced ACO Design model to succeed ACO REACH in 2027, signaling its continuing interest in value-based payment frameworks.
- The Gist: CMS continues to frame ACO participation as central to its strategy for whole-person care and cost management. Adoption, while not rapid, has been steady. For hospitals, this slow but sure transition toward value-based payment frameworks—two decades after value-based care was broadly introduced on a national scale—demands hard choices about strategic positioning and capabilities. There is progress in moving away from traditional fee-for-service toward value-based arrangements, including aligning financial risk with quality outcomes and integrating payment reforms into hospital operating models, but challenges remain. Value-based payment demands robust clinical analytics, risk management infrastructure and clarity on population health strategies to handle more complex payment regimes. The broader shift to value-based payment will not happen overnight and will coexist with legacy payment models, so health systems must continue to balance investment in new care models with pragmatism about current revenue drivers.
- Cyberattacks reach five-year Cyberattacks against healthcare organizations rose internationally in 2025, according to a report released last month. The report, from the health cybersecurity analysis company Health-ISAC, found a 21% increase in healthcare-specific incidents, with 575 cases in 2025, up from 476 in 2024. Across all industries, incidents rose from 5,744 in 2024 to 8,903 in 2025. The fourth quarter saw the highest level of healthcare ransomware of the year, with 190 attacks. About 80% of those incidents occurred in the Americas, but the report did not offer U.S.-specific data. The report urges healthcare organizations to take numerous steps to protect themselves against cyberattacks, such as implementing multifactor authentication and maintaining offline backups.
- The Gist: Cyberattacks remain one of the most serious threats facing hospitals and their patients. The latest data show these attacks continue to disrupt care and expose sensitive information. The FBI’s 2024 Internet Crime Report found that healthcare experienced more cyberattacks than any other critical infrastructure field. By the end of 2024, a record 259 million Americans had their health data compromised, including 192.7 million people affected by the Change Healthcare ransomware attack. Cyberattacks are unlikely to slow, and the scale of recent breaches should serve as a warning. It’s an expense that’s not going away. Hospitals must continue investing in stronger cybersecurity defenses, workforce training and continuous monitoring to safeguard operations.
And—what’re following.
- Federal health officials urged the public to vaccinate against measles as outbreaks surge across the country.
- A preliminary deal was struck for two-thirds of striking nurses as the New York City nurses’ strike reaches its fourth week.
- Approximately 3,000 Kaiser Permanente pharmacy and lab workers ended their three-day strike and are due to return to work this Thursday.
Plus—what we’ve been reading.
- Can AI bridge the primary care shortage? A recent KFF Health News article follows a Boston-area patient who turns to an AI-assisted virtual primary care platform following her primary care physician’s death. The patient could not find a nearby primary care physician without waiting at least a year and a half for an appointment. Fortunately, Mass General Brigham’s new AI-supported primary care program, Care Connect, met her needs in days. The platform uses an AI chatbot to collect symptoms and generate a clinical summary, which is reviewed by a remote physician who consults via video. The story considers the AI-enabled platform within the broader physician shortage. Critics charge that these platforms are only a bridge to timely access and do not replace traditional care provided in person by a physician.
- The Gist: The primary care physician shortage hampers patients’ ability to establish a trusting relationship with a dedicated clinician quickly. AI-enabled virtual primary care can serve as a bridge, expanding timely access and reducing delays. For patients shut out of traditional practices, these tools can address medical needs fast, reducing delayed care. But access is not the same as continuity. The difficult work of building trust and coordinating care still usually falls to the primary care physician. AI may buy time for now; whether it can replace the human side of care remains an open question.
Graphic of the Week
A key insight illustrated in infographic form.
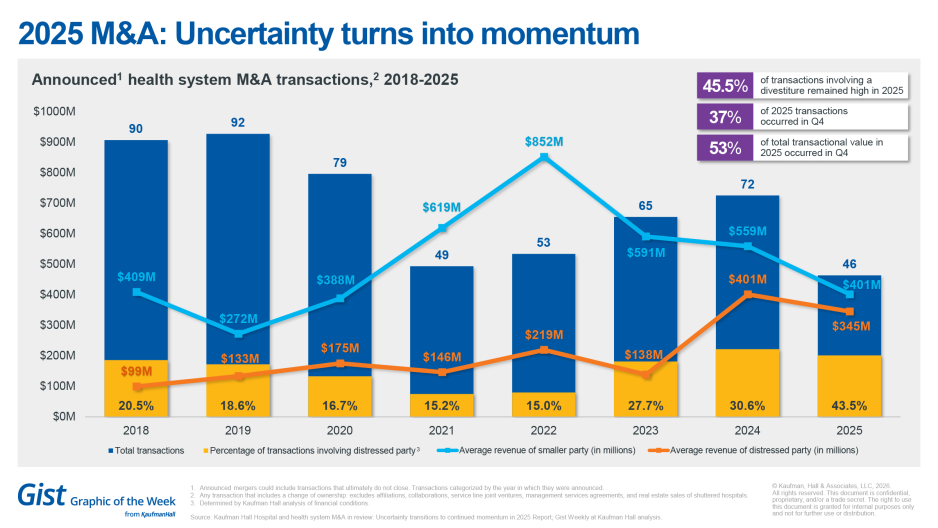
2025 M&A: From uncertainty to momentum
This week’s graphic highlights data from Kaufman Hall’s recently published 2025 Hospital and Health System M&A in Review on the dynamics in health system merger and acquisition (M&A) activity. The number of announced transactions reached record lows in the first and second quarters, and rebounded in the latter half of the year, bringing the total volume to 46. The average size of the smaller party involved in the transaction declined to $401M, a figure similar to pre-pandemic years. Notably, financial distress continues to be a driver of M&A activity. Distressed M&A activity reached an all-time high in 2025, with 43.5% of all transactions involving a distressed party. Additionally, 45.6% of announced transactions involved a divestiture. While all three rating agencies issued stable or neutral outlooks for 2025 and maintained these for 2026, the M&A landscape in 2026 continues to shift with ongoing portfolio rationalization, persistent financial headwinds and regulatory environment evolution.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Many perioperative improvement efforts stall—not because of poor execution, but because leaders focus on isolated metrics rather than the full perioperative system.
A new article explores how interdependent decisions across scheduling, staffing, block time and governance shape true performance—and how aligning these elements can improve access, efficiency and financial results.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
Last Monday, host J. Carlisle Larsen concluded her two-part conversation with Jesse Ehrenfeld, M.D., on physician mental health, examining how licensing rules, confidentiality concerns and medical culture can discourage doctors from seeking care, even as reform efforts gain momentum.
This Monday, rural America has lost more than 10% of its family physicians since 2017. What does that mean for access to care and for the communities left behind? We unpack the new data with Colleen Fogarty, M.D., Professor and Chair of Family Medicine at the University of Rochester.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thank you for reading! Please stay tuned for next week and check out our Gist Weekly archive for past editions. We also have our recent Graphics of the Week available here.
The Gist Weekly team at Kaufman Hall








