In the News
The biggest news of the week—and what we think about it.
- Patients struggle with the burdens of prior authorization. About seven in 10 insured adults consider prior authorizations a burden, according to a KFF poll published Monday. The poll found that one-third of patients find prior authorization a “major” burden and said experiencing denials and delays negatively affected their finances, stress and mental health. Prior authorization denials and delays also affected the physical health of about 26% of insured adults, the poll found. Meanwhile, four in 10 people living with chronic conditions said that prior authorizations are their single biggest healthcare burden beyond costs, with almost 60% saying that they have experienced denials, delays or requirements to seek alternative care.
- The Gist: Seeking approval before receiving recommended care is laborious, disruptive and costly. Prior authorization is especially common for Medicare Advantage (MA) enrollees, nearly all of whom must obtain prior authorization before some services, amounting to 53 million requests in 2024. By contrast, only 625,000 prior authorizations were sought for traditional Medicare enrollees that year. The Center for Medicare and Medicaid Innovation’s Wasteful and Inappropriate Service Reduction Model pilot project will use artificial intelligence to review some prior authorizations, but hospitals and patients are still concerned. To help address the prior authorization burden, some organizations are supporting a new bill that would influence how MA plans employ the practice. Health systems should evaluate how they can mitigate prior authorization with care coordination to avoid cancellations and lost revenue.
- Healthcare coverage tops list of Americans’ cost concerns. Healthcare expenses now outrank food and housing on the list of cost concerns for Americans, according to a KFF poll released last week. Two-thirds of survey respondents reported worrying about affording healthcare, and more than half said their health costs have risen this year and will continue to do so. One-third of respondents said they were “very worried” about healthcare bills, compared with less than 25% feeling the same way about food and housing. The poll also found that healthcare affordability will affect voters’ election decisions later this year. The poll findings come as Urban Institute analysts called this year’s premium increases an “aberration” compared with prior years.
- Gist: Following the expiration of the Affordable Care Act enhanced premium tax credits, coverage prices are rising—and the public’s worries are rising right along with them. Over a third of the public has reported missing or delaying care due to cost in the past year. The recent KFF poll results suggest this will worsen. The rising premiums are estimated to leave about 5 million without insurance and many others have opted for a lower-initial-cost, high-deductible bronze plan. An increase in delayed and uncompensated care may lie ahead. Hospitals have already been working to address cost concerns by pursuing strategic partnerships and are rethinking charity care and how patients are supported.
And—what we're following.
- Healthcare bankruptcy filings decreased 21% in 2025, declining for the second year in a row.
- The Centers for Medicare & Medicaid Services is considering ways to encourage hospitals to purchase supplies and medications made in the United States.
Plus—what we’ve been reading.
- Is precision medicine coming to obesity care? Published last month by National Public Radio, this article explains why GLP-1 drugs work well for some patients but not others, and how that reality may be about to push obesity care toward a more personalized, precision-medicine approach. Blockbuster GLP-1s (e.g., Ozempic, Wegovy) have reshaped obesity treatment and even show promise for treating addiction, attention-deficit/hyperactivity disorder and other conditions. But they are not a universal fix; while many patients experience significant weight loss, a sizable share sees limited benefit, struggles with side effects or gives up because of high prices and inconsistent insurance coverage. Obesity is biologically complex, with different genetic, endocrine and metabolic drivers influencing how patients respond. Researchers and clinicians are now trying to gauge which GLP-1 drug works best for each patient. This trial-and-error approach may be laying out the groundwork for a more precise model of obesity care.
- The Gist: GLP-1s are almost old news at this point; they are embedded into routine care and protocols for prescribing, monitoring and long-term management are usually in place. Applying concepts of personalized medicine to obesity care adds a new wrinkle. Systems will need to balance growing patient demand with inconsistent payer coverage and drug costs that remain stubbornly high, even if some of the pressures are showing signs of easing. Precision obesity care may also require better data infrastructure and closer coordination across primary care, endocrinology, nutrition services and other specialties. GLP-1s have already impacted care delivery and service volume across the system of care, making obesity management a core aspect of care rather than a niche program.
Graphic of the Week
A key insight illustrated in infographic form.
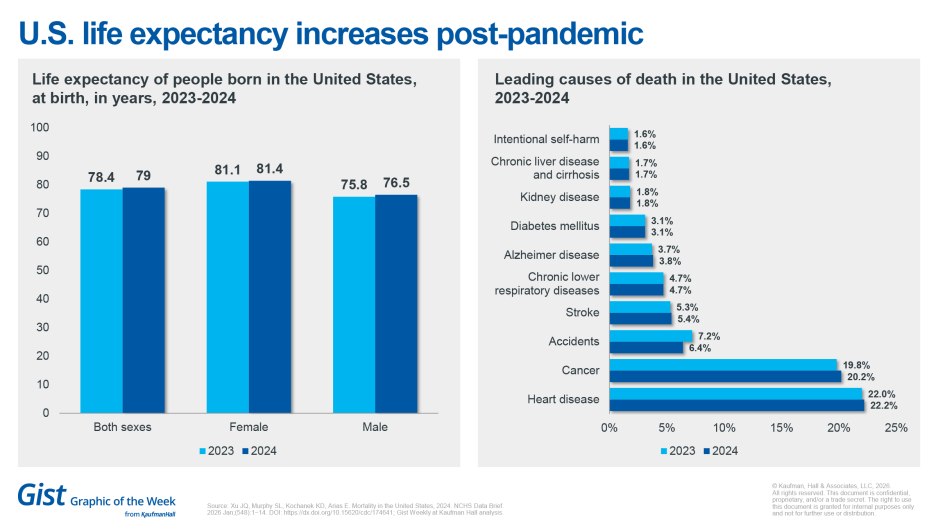
U.S. life expectancy increases post-pandemic
Life expectancy is rising, according to the latest Centers for Disease Control and Prevention release of U.S. mortality data. Life expectancy at birth increased to 79 years in 2024, up from 78.4 years in 2023. The leading causes of death remained largely the same as in 2023, but suicide replaced Covid as the 10th leading cause of death. Heart disease continues to prevail as the leading cause of death for people living in the United States.
This week at Kaufman Hall
What our experts are saying about key issues in healthcare.
The most significant constraint on healthcare performance today is not capital, technology or demand—it is workforce stability. What was once viewed as a workforce management issue has become a core enterprise risk, directly affecting quality, safety, access and margin. Persistent turnover, vacancies, burnout and leadership instability are no longer episodic challenges.
In a new article, Therese Fitzpatrick and Nikki Gruebling outline three mutually reinforcing actions that underpin the workforce strategy at high-performing health systems: keeping the workforce they have, building the workforce they need and optimizing the workforce they want.
On our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
Last Monday, we began a conversation on physician mental health with Jesse Ehrenfeld, M.D. In part one, we looked at why so many physicians struggle with depression and anxiety but never seek help, and how medical culture, stigma and long-standing expectations contribute to that silence.
This coming Monday, we continue the conversation, focusing on what happens when physicians do consider getting help. Dr. Ehrenfeld discusses concerns about licensing, confidentiality and other structural barriers that can make seeking mental healthcare feel risky, even as efforts to change those systems move forward.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thank you for reading! Please stay tuned for next week and check out our Gist Weekly archive for past editions. We also have our recent Graphics of the Week available here.
The Gist Weekly team at Kaufman Hall








