In the News
The biggest news of the year—and what we think about it.
- The healthcare AI train left the station. In 2025, healthcare emerged as one of the fastest adopters of artificial intelligence (AI) in the United States, even as reports released in October found that many AI pilots failed to demonstrate return on investment (ROI). As attention shifted toward agentic AI, persistent gaps in infrastructure and governance limited hospitals’ ability to move innovation beyond pilots and deliver broad impact. In June, the FDA released its approach to “unleashing” AI, followed in September by guidance from the Coalition for Health AI (CHAI) and the Joint Commission. In December, the Department of Health and Human Services (HHS) announced its own AI strategy to boost efficiency and modernization. Meanwhile, some policymakers and experts warned that incentives to deploy AI may be advancing faster than regulatory safeguards.
- The Gist: Hospitals are under constant pressure to compete for and deliver value to patients and remain financially sustainable. Many hospitals will continue to turn to AI for help—but only if they can trust it. Many AI pilots have fallen short, which suggests that technology cannot fix broken workflows or other serious concerns without strong data infrastructure and governance. Recent moves suggest progress toward the guardrails and guidance that is needed to build confidence and scale AI responsibly. All things considered, AI adoption is likely to become table stakes for healthcare providers in the future—if regulators, providers and vendors align around safety, value measurement and responsible deployment.
- What a year for federal health policy! President Trump put his stamp on health policy immediately following his January inauguration—beginning to withdraw from the World Health Organization and rescinding some of President Biden’s healthcare-related executive orders right away. Executive orders and adjustments to the Affordable Care Act (ACA) followed, but that was only prelude to some of the bigger changes that were to come. Significant staff cuts and restructuring were announced for HHS. HHS Secretary Robert F. Kennedy Jr. announced in June that he would replace the entire Advisory Committee on Immunization Practices, a Centers for Disease Control and Prevention panel that makes recommendations on vaccines to inform the vaccine schedule and coverage. This action preceded significant revision to the federal vaccine schedule, which did not go over well with some professional societies. Meanwhile, the president followed through on his campaign promise to raise tariffs, although not without reservations complicating long-term planning. On the legislative front, the One Big Beautiful Bill (OBBB) was passed and signed in July; the law includes an estimated $1.06 trillion in healthcare spending cuts over the next decade.
- The Gist: To call 2025 a momentous year for federal health policy would be an understatement. The impact of the legislative and regulatory changes this year brought will be felt for years, if not decades. The OBBB will likely have the most significant long-term impact on hospitals, highlighted by major changes to the Medicaid program including to the provider tax safe harbor, caps on state directed payments, enhanced eligibility requirements and work requirements for able-bodied adults. Further, the Congressional Budget Office estimates that by 2034, approximately 10 million Americans will have lost health coverage. As 2025 came to a close, the House of Representatives could not find a way to extend ACA enhanced tax credits, which—unless Congress steps in in January—likely means that millions of Americans may face steep premium increases or go without health insurance altogether. This would surely be a lump of coal for consumers struggling with affordability and for hospitals facing the unhappy prospect of uninsured patients at their doorstep.
- The end of an era for health plans? Health insurers faced mounting financial and regulatory pressure throughout 2025, in a turnabout from their heady days just a few years ago. In January, Moody’s Ratings downgraded its sector outlook, citing growing political and financial scrutiny of insurers and pharmacy benefit managers (PBMs) amid wavering public trust. UnitedHealth Group, long viewed as the industry’s most resilient player due to its scale and vertical integration faced mounting pressure as it reported earnings misses, shifted guidance, disclosed federal investigations and announced exits from select Medicare Advantage markets. In December, Fitch Ratings issued a deteriorating outlook for insurers in 2026, pointing to sustained cost pressure across multiple business lines.
- The Gist: Despite the industry’s enormous scale, the data point to an inflection: the golden era of health plans appears to be ending. Rising medical costs, regulatory scrutiny and political pressure are compressing margins and eroding predictability. As margins tighten, even as premiums increase, payers are likely to lean more heavily on aggressive rate negotiations, tighter contract terms and greater risk transfer to right their ships. For providers and employers, this sets the stage for tougher, more protracted negotiations and a less forgiving reimbursement environment. The next chapter for health plans will be defined not by growth at any cost, but by margin defense in a far more constrained operating landscape.
Graphic of the Year
This year’s most popular insight illustrated in infographic form.
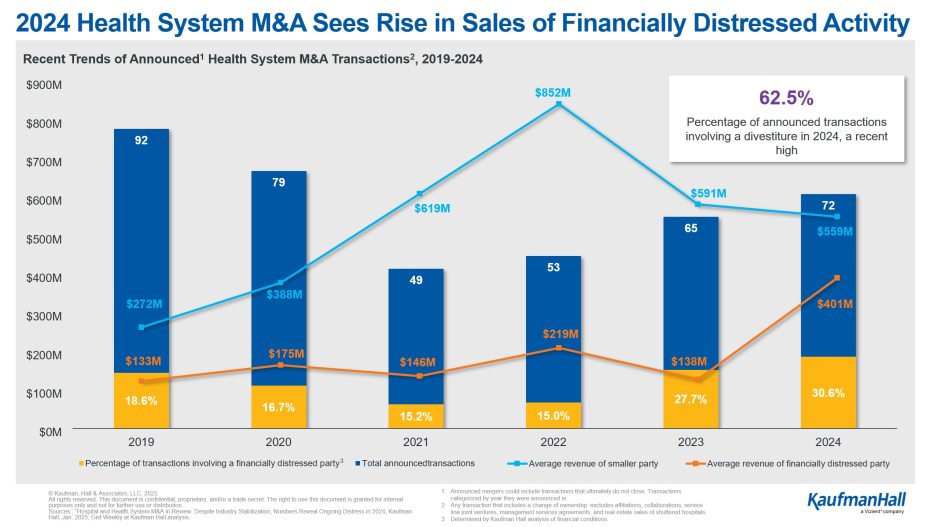
2024 Hospital M&A signaled early optimism for 2025
Published in January, the Graphic of the Year highlighted data from Kaufman Hall’s 2024 Hospital and Health System M&A in Review, capturing a sector cautiously emerging from post-pandemic disruption. With 72 announced transactions in 2024, health system merger and acquisition activity began ticking back up toward pre-pandemic levels. In 2025, a slow first half of M&A activity took place in the shadow of macro-economic volatility and uncertainty prior to the OBBB’s passage. However, third quarter transactions trended upward and are more in line with historical trends, according to Kaufman Hall’s Q3 M&A Quarterly Activity Report.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
As providers grappled with the developments explored above for much of 2025, our Kaufman Hall team observed a somewhat surprising trend: a re-embrace of enterprise strategy by a number of midsized, independent health systems.
A new blog explores how health system leaders carefully evaluated growth initiatives, advanced ambulatory and service line efforts, and balanced performance improvement, growth, and transformation activities throughout 2025.
The authors also share their predictions for health system strategy in 2026—including the imperative for transformation to better serve their missions.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
As 2025 comes to a close, Gist Healthcare Podcast host J. Carlisle Larsen was tasked with selecting a few standout conversations from the year. She offers this:
My initial reaction was to include all of them. I am fortunate to engage in thoughtful, engaging and at times challenging discussions with leaders, clinicians, journalists, academics and others. Each conversation this year reflected a commitment to making healthcare better.
Early in the year, I spoke with Bruce Siegel, M.D., M.P.H., president and CEO of America’s Essential Hospitals, about anticipated changes to how the federal government may implement and fund the Medicaid program. At the time, the outlook was uncertain, but our discussion focused on how potential funding reductions could affect safety-net hospitals nationwide. In hindsight, the conversation feels prescient, as we await the long-term effects of the One Big Beautiful Bill, which passed in July and will influence healthcare policy for years.
We must acknowledge the rapid advancement of artificial intelligence and its growing adoption across healthcare organizations. While interest in these tools accelerate, clear and consistent guardrails remain limited. This summer, I spoke with Brian Anderson, MD, CEO of the Coalition for Health AI, as the organization announced a partnership with The Joint Commission to develop best practices for scaling AI in healthcare. Over the course of our two-part conversation, we explored how insights from hospitals are shaping recommendations and informing the future use of AI across health systems.
I also want to highlight my conversation with Sylvia Owusu-Ansah, M.D., associate professor of pediatrics and emergency medicine at the University of Pittsburgh School of Medicine and director of EMS at UPMC Children’s Hospital of Pittsburgh. Dr. Owusu-Ansah served as a medical advisor to the HBO medical drama The Pitt, which has been praised for its realistic portrayal of emergency department care over the course of a single shift. Our discussion offered a unique perspective on seeing real-world clinical experiences brought to life on screen.
2025 was a momentous year in healthcare, and there is every reason that 2026 will be just as busy. I look forward to sharing upcoming conversations on physician mental health, the expanding role of advanced practice providers and anticipated regulatory changes.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thank you for reading! The Gist will be on hiatus for the remainder of the year. We’ll see you next year on January 9, 2026! In the meantime, please check out our Gist Weekly archive for past editions. We also have our recent Graphics of the Week available here.
Merry Gistmas and warm wishes to all!
The Gist Weekly team at Kaufman Hall