From the Gist Weekly team at Kaufman Hall, a Vizient company
In the News
What happened in healthcare recently — and what we think about it.
- OBBB may trigger Medicare cuts: CBO. The One Big Beautiful Bill (OBBB) could reduce Medicare spending by nearly $491 billion between 2027 and 2034, the Congressional Budget Office (CBO) said in a letter last week. The CBO, in response to an inquiry from congressional Democrats, outlined the process that would determine whether the OBBB triggers statutory pay-as-you-go requirements. The cuts would be triggered if the White House’s Office of Management and Budget (OMB) estimates that the OBBB adds to the deficit over a 5- and 10-year period, a determination OMB has not yet made. According to the CBO’s estimates, Medicare would face a $45 billion reduction in 2026, rising to roughly $76 billion by 2034.
- The Gist: Unless Congress intervenes, an estimated 4% across-the-board reduction in Medicare spending will begin next year. The combination of nearly $500 billion in Medicare cuts with the OBBB’s tightening of Medicaid eligibility and the potential rollback of Affordable Care Act tax credits adds up to a serious budget headache. The CBO has already estimated that the OBBB may leave 10 million more uninsured by 2034, further stressing providers. This may be familiar territory to hospitals, which have weathered disruptions before, but the landscape has changed. Flourishing in the face of uncertainty will require a focus on four imperatives: margin transformation, care delivery realignment, structural resilience and technological enablement. Hospitals will need to be nimble enough to realign care delivery models, lean into digital tools and fortify financial resilience when needed.
- Employers foresee major healthcare cost hikes in 2026, survey says. Large companies are bracing for a 9% jump in healthcare costs next year, a new survey found. The survey was published Tuesday by the Business Group on Health, a coalition comprising 121 large employers insuring 11.6 million people. It finds a “troubling dynamic” in which employers are planning for one of the steepest increases in healthcare costs in more than a decade. Even with plan design changes, employers anticipate costs will rise by about 7.6%. They cite GLP-1s and other high-cost drugs, along with general medical inflation, as the main drivers. To contain spending, many employers are considering higher employee cost-sharing, tougher utilization management and new approaches to pharmacy benefit management.
- The Gist: Employers already started off 2025 at a disadvantage after experiencing steep cost increases over the past two years. For hospitals, the survey signals more cost sensitivity ahead. Rising deductibles and premiums make it more likely patients will delay elective care or skip follow-up visits altogether. Employers’ push for affordability also likely means narrower networks and more, or tighter, partnerships with providers they deem to be of high value. Hospitals that can demonstrate strong outcomes, care coordination and competitive pricing will be positioned to stay in those networks, while others risk being steered away.
- AAP releases its own vaccine guidelines, counter to HHS. The American Academy of Pediatrics on Tuesday published its own childhood immunization schedule, with guidance diverging from that of federal health leaders. The schedule covers 18 diseases, including Covid-19, measles and flu. The move comes after Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. removed members of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices and installed new appointees to the panel, which traditionally shapes guidelines on routine vaccinations. This marks the first time in 30 years that the AAP has substantially diverged from federal guidance since AAP started syncing its advice with the federal government’s. The AAP emphasized that its recommendations are grounded in scientific evidence and focused on child health, but Kennedy criticized the AAP on social media and an HHS spokesman accused the group of “freelancing its own recommendations.”
- The Gist: Traditionally, the federal government issues immunization schedules, and payers align coverage decisions with those standards. The introduction of competing guidelines from a leading medical society creates the potential for confusion among patients and insurers. Hospitals may face operational challenges if payer policies diverge from physician recommendations, including inconsistencies in coverage and reimbursement. The AAP’s move comes as an independent, ad-hoc coalition of physicians and researchers known as the Vaccine Integrity Project reaffirmed the safety and effectiveness of vaccines for Covid, RSV and influenza, further highlighting the divide between federal policy and medical consensus. These conflicts complicate communications with patients and families, who look to both clinicians and insurers for clear guidance. Hospitals are likely to be caught between medical best practice and administrative realities.
Plus — what we’ve been reading.
- Living longer with cancer. Published earlier this month in The Wall Street Journal, this story details how a new generation of cancer treatments is extending life for people once given only months to live. It tells the story of Gwen Orilio, diagnosed with Stage 4 lung cancer in her early 30s, who has lived more than a decade through successive lines of therapy targeting genetic mutations. Her case reflects a broader trend: Patients with metastatic cancers such as of the lung, breast, melanoma and kidney are living longer (as much as a decade or more) but are rarely cured. Federal data show survival rates for advanced cancers climbing as targeted therapies and immunotherapies expand. But the shift has created new challenges, from ongoing side effects and financial strain to the emotional toll of repeated scans and the uncertainty of when current drugs will fail. Researchers say the United States now has nearly 700,000 people living with Stage 4 cancers, a population projected to grow sharply.
- The Gist: For hospitals, the shift toward treating advanced cancer as a chronic condition means longer, resource-intensive relationships with patients. As care delivery moves from episodic interventions to sustained management, success will be measured not just in survival but in whether treatment aligns with patients’ goals and quality of life. The demand is partly extending survival, partly helping patients manage the weight of perpetual uncertainty. For patients, this evolution offers more time but also constant uncertainty: There is no cure, and the optimism is tempered by new considerations to be made. This prolonged limbo is becoming the new face of survivorship.
Graphic of the Week
A key insight illustrated in infographic form.
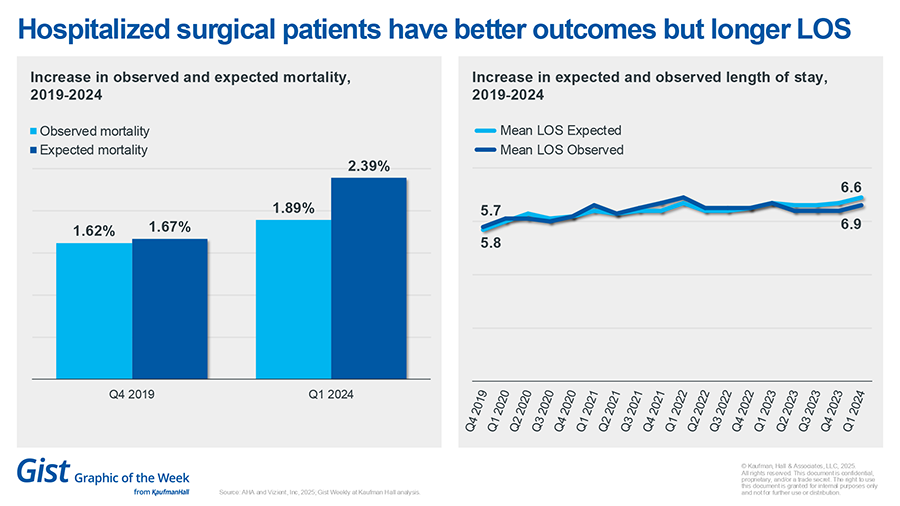
Better outcomes for surgical patients
A new report shows that the difference between expected and observed mortality rates for hospitalized surgical patients continues to improve. Hospitals have achieved nearly a 20% increase in survival rates for these patients compared with expected, reflecting advances in evidence-based care and safety practices. However, the analysis, from Vizient and the American Hospital Association, also finds that the average length of stay has risen by almost a full day over the past five years, due to increasing patient acuity and insurer-related delays in post-acute care placement, particularly in Medicare Advantage plans. This trend suggests ongoing challenges in balancing improved patient outcomes with efficient hospital throughput.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Hospitals often lose efficiency and money when physicians and advanced practice providers (APPs) are credited for the same work while the system carries APP costs.
In a new article, Bonnie Proulx urges a role-based framework that aligns incentives, scope and compensation through clear APP archetypes. She demonstrates how a targeted deployment of APPs can lift productivity significantly and swing margins from a loss to a gain.
On Our Podcast
The Gist Healthcare Podcast — all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
Coming up, a federal judge has vacated a Biden-era rule that would have more tightly regulated Medicare Advantage marketing. We get that story and the latest healthcare business and policy news, in 10 minutes or less, on Monday.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thanks for reading! The Gist Weekly will take a hiatus from publishing next week in front of the Labor Day holiday. We’ll be back on Friday, Sept. 5, with a new edition. See you then!
Best regards,
The Gist Weekly team at Kaufman Hall