Hello, and welcome to this week’s edition of the Gist Weekly. We are grateful for your continued readership. Please forward this email to friends and colleagues and encourage them to subscribe!
In the News
What happened in healthcare recently—and what we think about it.
- Site neutrality, hospital price transparency in new Medicare proposed rule. The Centers for Medicare & Medicaid Services (CMS) proposed a 2.4% payment increase for hospital outpatient departments and ambulatory surgical centers (ASCs) in 2026, alongside a series of policy changes that advance site neutrality. The proposal would expand site-neutral reimbursement for some services and begin phasing out the inpatient-only list, allowing more procedures to be paid at outpatient rates. Hospitals also would face tighter price transparency requirements, including mandatory machine-readable files and enhanced consumer-facing tools. Physicians would see a 3.8% payment increase under the Physician Fee Schedule, with targeted support for primary care specialties. CMS also is proposing new billing codes to support remote patient monitoring and digital therapeutics, signaling an effort to integrate more technology-enabled care. The combined changes reflect a continued shift toward uniform payment policies across care settings.
- The Gist: The proposed payment rules signal a deeper push toward cost containment and care standardization across settings. But site neutrality poses a major challenge for traditional health systems. It would equalize payment for services regardless of location, putting pressure on hospitals that operate under stricter regulatory requirements and higher fixed costs. At the same time, CMS is moving to eliminate the inpatient-only list, allowing more procedures to be reimbursed in outpatient settings, which could further shift volume and revenue away from traditional inpatient care. The expanded price transparency mandates, including enhanced requirements for machine-readable files and patient-friendly comparison tools, could increase demands on compliance and data systems. For physicians, a proposed 3.8% pay bump and new billing codes for digital therapeutics and remote monitoring suggest CMS is trying to support primary care and technology-enabled care delivery. Collectively, these changes favor lower-cost, flexible and tech-forward care models. These might save taxpayer dollars, but may come at the expense of health systems that have long been the backbone of community health infrastructure.
- Medical debt to remain on credit reports. Roughly 15 million Americans hoping their medical debt might be removed from their credit reports are now out of luck after a federal judge scrapped the Biden administration’s debt relief rule. The ruling, which was considered a blow to the Consumer Financial Protection Bureau, overturns a rule that would have erased $49 billion in medical debt and boosted credit scores by an average of 20 points. A Texas judge ruled the agency had overstepped its authority under the Fair Credit Reporting Act. Credit bureaus and financial industry groups cheered the decision, but consumer advocates warned the ruling will continue to penalize patients for circumstances beyond their control and widen financial and health disparities.
- The Gist: Disputes between insurers and hospitals lie at the root of a significant number of surprise bills, resulting in bad debt for patients. The decision to keep medical debt on credit reports could increase uncompensated care for hospitals. This may present an opportunity for hospitals to reexamine their charity care practices. At the same time, while this decision may increase debt collection, providers also may risk reputational harm by leaning more on third-party collectors. It is estimated that 1 in 12 U.S. adults carries unpaid medical bills of at least $250, and medical debt disproportionately affects lower-income and minority communities. Hospitals may face growing pressure to advocate for fairer billing and credit practices, and some systems have chosen to forgo adverse credit reporting of outstanding patient bills.
- Healthcare data breaches up 20% in 2025, report finds. A new report reveals that healthcare experienced 283 data breaches during the first 6 months of 2025, up from 236 in the same period of 2024, marking a 20% increase. These incidents impacted more than 16.6 million individuals, making healthcare the second most-targeted industry, behind financial services, according to the report published Wednesday by the Identity Theft Resource Center. Nationwide, 1,732 breaches were reported across all sectors, with cyberattacks causing 1,348 of them. Major incidents included Yale New Haven Health (5.56 million records), Episource (5.42 million records) and Blue Shield of California (4.7 million records). Nearly 70% of healthcare breach notices did not disclose the cause of the incident.
- The Gist: For hospitals and health systems, the surge in data breaches underscores the urgent need to strengthen cybersecurity infrastructure and incident response plans. With patient trust and regulatory compliance on the line, organizations must regard cybersecurity as a board-level risk. Major breaches at Change Healthcare and Oracle Health have made news, but this is clearly a broad, industry-wide problem. As cyberattacks, including attacks targeting biomedical equipment, grow more frequent and sophisticated, proactive investment in cybersecurity talent, tools and governance should be considered mission critical.
Plus—what we’ve been reading.
- Stopping Alzheimer’s before it appears. Published in June in The Wall Street Journal, this article tells the story of a family with a rare genetic mutation for early-onset Alzheimer’s as they enroll in a clinical trial. The Richardson family carries PSEN1, which has an early-onset, aggressive and predictable pattern of disease progression, unlike most forms of Alzheimer’s. The clinical trial explores the use of anti-amyloid drugs—the only FDA-approved drugs for Alzheimer’s—as preemptive therapy to delay and ultimately cut the risk of disease by half before symptoms appear. The children, who face a 50% risk of developing this disease, weighed the risks of side effects like brain swelling and bleeding—some of which have already occurred in study participants—before enrolling.
- The Gist: Few diagnoses are more frightening to patients and their families than Alzheimer’s. Many factors cause the disease, with more than 300 hereditary gene mutations responsible for just 1% of cases. PSEN1 is a mutation with predictable disease progression, making it an excellent candidate for research and drug development. Remternetug, the experimental anti-amyloid antibody studied in the clinical trial involving the Richardson family, is in the same class of drugs approved in recent years under the Food and Drug Administration’s Accelerated Approval Pathway. But they are not without controversy; serious side effects remain a concern as approvals rely on short-term trials with limited understanding of long-term outcomes. The use of Remternetug, manufactured by Eli Lilly, as a preventive measure before amyloid plaques appear is even more speculative and experimental than other drugs approved in its class. While several Alzheimer’s medications recently have been approved, concerns remain about their long-term risks and effectiveness.
Graphic of the Week
A key insight illustrated in infographic form.
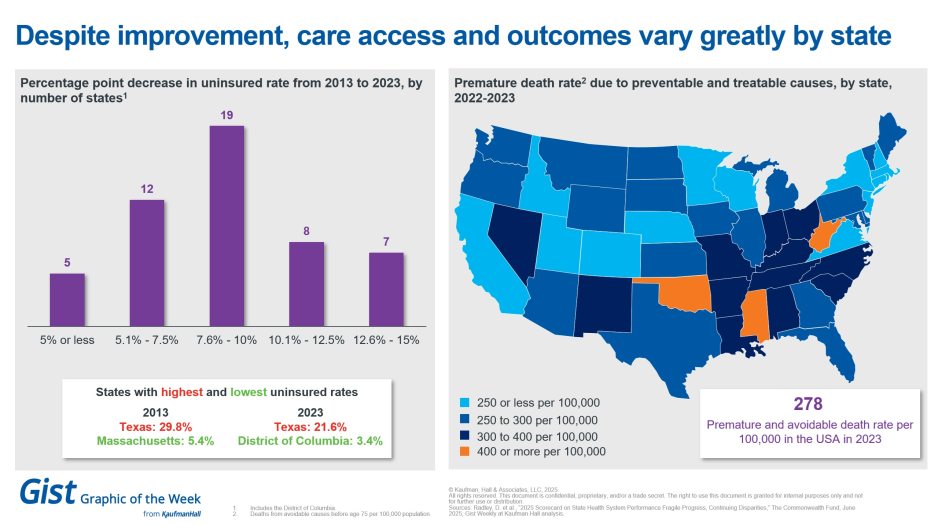
A deep dive into state health scorecards
This week’s graphic highlights a new report from The Commonwealth Fund with data on state-by-state health performance. The good news is that all states have seen a drop in their uninsured rate between 2013 and 2023, and the gap between the most- and least-insured states is shrinking. Texas had the highest uninsured rate in both years, but its rate dropped by 27.8%. However, there remains significant variation in preventable deaths by state. The report ranks states on 50 measures of healthcare access and affordability, prevention and treatment, avoidable hospital use and costs, health outcomes and healthy behaviors, and other factors. It finds that the infant mortality rate worsened in 20 states between 2018 and 2022, with considerable variation across states. This snapshot-in-time report calls for targeted, coordinated federal and state policies to raise health system performance across the nation.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Physician practices may neglect succession planning until it’s too late, but those that start preparing well in advance are positioned to continue growing, attract top talent and serve their communities effectively.
A new special report by Walter Morrissey and Nora Kelly explores the challenges and the opportunities in structured succession planning. One key finding: proactive succession planning enables practices to maintain stability, preserve institutional knowledge and ensure uninterrupted patient care while minimizing risk during leadership transitions.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
Last Monday, Gist Healthcare Podcast host J. Carlisle Larsen spoke with Michael McAuliff of Modern Healthcare to talk more about the passage of the One Big Beautiful Bill Act.
The mental health of nurses is a priority for hospitals. This coming Monday, JC is joined by BayCare Health System’s Chief Nurse Executive Trish Shucoski and Rocky Hauch, an advanced nursing educator for the system, about their successful nurse wellbeing pilot being rolled out to all 16 BayCare hospitals.
To stay up to date, tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thanks for reading! We’ll see you next Friday with a new edition. In the meantime, check out our Gist Weekly archive if you’d like to review past editions. We also have all of our recent “Graphics of the Week” available here.
Best regards,
The Gist Weekly team at Kaufman Hall, a Vizient company








