From the Gist Weekly team at Kaufman Hall, a Vizient company
In the News
What happened in healthcare recently — and what we think about it.
- With chaos at the CDC, states go their own way on vaccines. Confusion surrounding national vaccine guidance has prompted some states to issue their own guidelines and retailers to rethink in-store policies. With Susan Monarez, director of the Centers for Disease Control and Prevention (CDC), pushed out after just a month on the job, a leadership vacuum has emerged as the new acting director assumes the helm of the nation’s public health agency and several high-ranking officials have resigned in protest. As the CDC’s turmoil persists, its Advisory Committee for Immunization Practices — which develops vaccine recommendations and is now led by a prominent vaccine skeptic — is set to meet later this month, despite criticism from Republican Sen. Bill Cassidy, a Louisiana physician concerned about protecting access to vaccines. Meanwhile, the Food and Drug Administration (FDA) narrowed its approval for Covid-19 vaccines, making it more difficult for younger, healthy people to get the shot. This comes even as Covid cases surge in some states. While President Trump has expressed sympathy for the anti-vaccination movement and support for Health and Human Services Secretary (HHS) Secretary Robert F. Kennedy Jr., he has also praised Covid vaccine success, citing “great numbers and results.”
- The Gist: It has been a dizzying few weeks for HHS and its agencies, particularly the CDC, and consequently for the nation’s vaccine policy. Hospitals can be forgiven for not knowing what the latest guidance is, because it is changing so rapidly and there is so much conflicting advice. Typically, the FDA approves vaccines, the CDC recommends a schedule, and providers and commercial payers follow these recommendations in their treatment and coverage decisions. But the old playbook has been tossed out the window — at least for now. Some states are actively going further than the CDC’s recommendations; at the other end of the spectrum, Florida has taken steps to eliminate vaccine requirements for schoolchildren. Private medical societies also are diverging from federal guidance, further clouding the vaccine waters. Lawmakers from both parties are losing patience with the apparent turmoil, but Kennedy is not backing down, nor does he need to, thanks to continued White House support. With so much up in the air and so much potential for confusion, hospitals need to pay close attention to their state laws and regulations and try to provide clear answers to patients who may need new prescriptions for vaccines.
- Medicare experiments with prior authorization. The Centers for Medicare & Medicaid Services (CMS) has announced a pilot program to test prior authorization for traditional Medicare. The pilot, Wasteful and Inappropriate Service Reduction (dubbed the WISeR model), begins Jan. 1, 2026, in six states — New Jersey, Ohio, Oklahoma, Texas, Arizona and Washington — and lasts for six years. The WISeR model imposes prior‑authorization requirements for 17 outpatient services, including skin and tissue substitutes, nerve‑stimulator implants and knee arthroscopy. Private vendors will use artificial intelligence to determine whether patients would be covered for some procedures. Critics have charged that financial incentives tied to reducing service utilization could skew decisions.
- The Gist: This marks a major departure from the fee-for-service model of traditional Medicare, aligning it more closely with a practice commonly used in Medicare Advantage, but with an AI‑assisted review. Licensed providers will make final calls, but AI tools will help sift requests, and providers can choose pre‑service authorization or face post‑service review and potential non‑payment. WISeR may erode traditional Medicare's long‑standing appeal of fewer barriers. If the program succeeds in cutting waste without cutting care, it could be a win for taxpayers — but only if CMS meticulously monitors delays, denials and patient outcomes. Particularly in the affected states but more broadly speaking nationwide, hospitals will need to watch this carefully, or they will scramble under the weight of new administrative burdens and angry patients.
Plus — what we’ve been reading.
- No doctors in the ED. Published in August by KFF Health News, this story profiles Dahl Memorial, a small hospital in rural Ekalaka, MT, operating an emergency department (ED) without an on-site physician. Dahl Memorial is one of a growing number of rural EDs that rely on physician assistants and nurse practitioners to stabilize patients and coordinate transfers for higher-level care, often without a doctor ever being present. This approach is becoming more common among low-volume critical access hospitals, although it varies by state. A recent study found that in 2022, at least 7.4% of EDs across the United States did not have an attending physician on-site 24/7. Like Dahl Memorial, more than 90% were in low-volume or critical access hospitals.
- The Gist: Non-physician rural EDs are a staffing reality shaped more by necessity than design. Hospitals are striking a balance by using advanced practice providers with emergency training and remote backup to keep doors open in areas where physician recruitment is difficult. At least three states have passed laws mandating round-the-clock physician coverage, but many others have not. These mandates raise real questions: if hospitals can’t comply, what will happen next? Meanwhile, nearly half of the EDs in Montana and the Dakotas operate without doctors — and none of those states has an ED residency program.
Graphic of the Week
A key insight illustrated in infographic form.
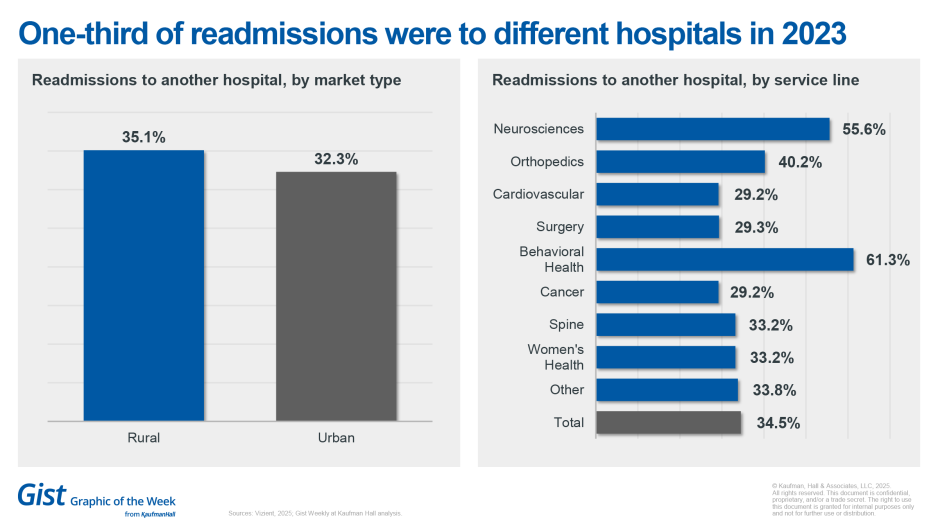
Behavioral health, neurosciences lead different-hospital readmissions
One-third of discharged patients go to a different hospital when requiring a readmission, according to data from Vizient’s CMS Qualified Entity Public Report, published last month. The highest proportion of different-hospital readmissions were for behavioral health (61.3%) and neurosciences (55.6%). Readmission rates were higher in urban areas (16.7%) than rural areas (15.4%), but rural patients were more likely to be readmitted to a different hospital, 35.1% vs. 32.3% for patients residing in urban areas. These “invisible returns” complicate care coordination and outcome tracking. Such fragmentation disproportionately affects high-risk populations, particularly those in vulnerable areas (as measured by the Vizient Vulnerability Index) and those covered by Medicaid or Medicare. The implications for patient retention are clear: if patients aren’t satisfied with the treatment at your hospital, they’ll go somewhere else.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Service lines are back in fashion, but the return of service lines isn’t a nostalgia play. Under unrelenting market pressures and increasing strategic complexity, health systems are embracing service lines as a tool for driving growth for systems and care coordination for patients.
In a new article, Kaufman Hall’s Walter Morrissey and Sg2’s Chad Giese discuss the evolution of service lines into strategic, enterprise-wide platforms to deliver value. They also discuss the five dimensions of success for the new service line model that provide a practical framework for the tough decisions health systems must make around their service-line strategy.
On Our Podcast
The Gist Healthcare Podcast — all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
The podcast will be on hiatus for a few days starting next Monday. We will return with the latest healthcare business and policy news, including a new study that finds that fewer than one in three adolescents with opioid use disorder received substance use disorder treatment. That’s coming up on Wednesday, September 17.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Best regards,
The Gist Weekly team at Kaufman Hall








