In the News
What happened in healthcare recently—and what we think about it.
- Trump, FDA jump into Tylenol debate. President Trump this week publicly urged pregnant women to avoid using Tylenol (acetaminophen), claiming a link between its prenatal use and autism in children. He made the statement at a White House event in which he argued that Tylenol and childhood vaccines could be contributing to rising autism rates, as the Food and Drug Administration (FDA) issued new official guidance on a possible link. Tylenol’s manufacturer, Kenvue, has repeatedly denied the claim. President Trump’s remarks and the new FDA guidance were immediately challenged by major medical organizations, which noted that existing studies show some correlations but not causation, and that acetaminophen remains one of the few safe options during pregnancy for reducing fever or pain.
- The Gist: For hospitals, the fallout could be significant. Care teams may face increased patient anxiety and pressure to justify or defend standard pain-and-fever protocols, especially for expecting parents. The new guidance could drive demands for untested alternative therapies or lead to avoidance of clinically indicated acetaminophen use, which risks leaving fevers—a known fetal hazard—untreated. In the vacuum created by unclear guidance from the federal government, professional societies will intensify efforts to promote clear communication, and hospital risk managers may need to prepare guidance and internal FAQs to help clinicians respond.
- Last-minute scramble as millions brace for ACA sticker shock. House Republicans have introduced a bill to extend the enhanced Affordable Care Act premium tax credits for one year, a move aimed at averting steep coverage losses if the subsidies expire. The bill comes as the deadline looms; as many as 24 million Americans could see their health coverage costs skyrocket if Congress does not extend the tax credits, which are set to expire at the end of this year. It reflects growing concern that allowing the subsidies to lapse could create political backlash. Democrats are pressing for a permanent extension, but negotiations have been hampered by cost considerations and a tight legislative calendar. Some analyses project rate hike increases of 75% or more. The Congressional Budget Office has further warned that delaying a decision beyond September 30 will limit opportunities to reduce premiums and may accelerate coverage losses across the exchanges.
- The Gist: Hospitals could feel the effects almost immediately if subsidies lapse. When coverage becomes unaffordable, patients often forgo primary and preventive care, leading to higher rates of delayed treatment and reliance on emergency departments. That shift strains safety-net services and increases bad debt while also affecting payer mix, ultimately cutting into margin. Beyond the financial risks, hospitals may need to strengthen community outreach to help patients navigate coverage options and avoid lapses.
- Healthcare cyberattacks increasingly routine, expensive. Nearly half of U.S. healthcare organizations suffered a cybersecurity incident in the past year, and the number losing more than $200,000 from those breaches has surged by 400%, a new report has found. The report, from the cybersecurity firm Netwrix, found that losses topping $500,000 also rose sharply, hitting 12% of organizations compared with just 2% the year before. Attackers most often gained access through compromised credentials, with phishing and social engineering identified as leading tactics. The report warns that the growing use of AI by hackers is widening the gap between attackers and defenders.
- The Gist: Cybersecurity is no longer an occasional disruption. It’s a permanent reality that requires proactive planning and investment. Breaches are inevitable, with their fallout reaching beyond the direct cost to regulatory fines, reputational damage, the erosion of patient trust and even potential downgrades in bond ratings. For hospitals, that means treating cybersecurity not as a variable shock but as a fixed expense embedded in core operations. Strategic strength comes from building resilience across legal, compliance, IT and clinical teams and ensuring defenses, from identity management and phishing protection to monitoring and response, are consistently tested and reinforced. The question isn’t whether a breach will come, but whether your system is positioned to withstand the impact.
Plus—what we’ve been reading.
- Sometimes, cash might beat coverage. Pregnant patients are in some instances better off bypassing insurance when paying for prenatal genetic tests, according to a recent NPR article. The piece tells the story of a Miami resident who was billed $750 after Natera, a cell-free DNA testing provider, charged her insurer $4,480 for a blood test—of which insurance paid just 45 cents. Buried in her records was an earlier offer from Natera to instead pay a $349 “prompt-pay cash price.” A Reddit tip led her to request the cash rate retroactively, saving $400. Researchers note this dynamic is increasingly visible since price transparency rules took effect. In some instances, consumers paying cash can get a better rate than what insurers negotiate. Natera officials defended their practice as giving patients choice, though lawsuits have challenged its billing. For the patient, the experience changed her approach: she now questions every medical bill.
- The Gist: Patients tend to have difficulty understanding the cost of their care, despite laws and rules that support price transparency. A significant share of patients who are price-sensitive and concerned about affording their healthcare now search for prices and negotiate with providers about costs before seeking care. Their pre-clinical journey is increasingly digital, searching online to fill in gaps. Yet even with more options and retail-style entrants, navigating coverage and reimbursement remains complex. Cash pricing adds another layer, exposing a structural quirk of coverage: insured patients may pay more than those without. Patients are responding by price-shopping, negotiating, delaying care and making trade-offs to save money. As consumer choice expands and transparency becomes more common, competing on price may be critical to remaining relevant to patients worried about their increasing cost-sharing burden.
Graphic of the Week
A key insight illustrated in infographic form.
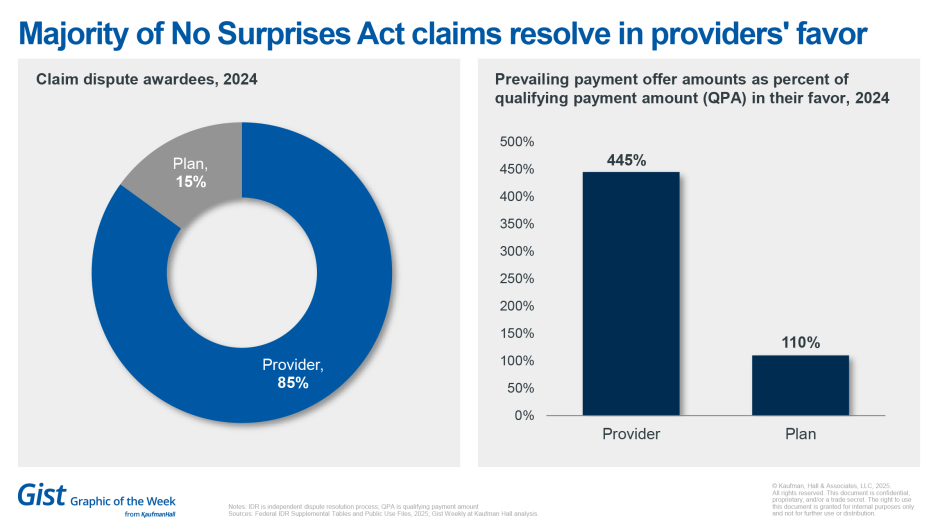
Providers prevailing in No Surprises Act disputes
Providers win the overwhelming majority of claim disputes under the No Surprises Act, prevailing 85% of the time in 2024, up from 81% in 2023, according to data recently published in Health Affairs. The data also show providers are winning substantial offer amounts—a median of 445% of the qualifying payment amount in 2024 (i.e., about 4.5 times what the insurer’s in-network equivalent would have paid), up from a median 327% in 2023. The data show the law’s arbitration mechanism incurring substantial costs—an estimated $5 billion from 2022 to 2024. The volume of disputes has exceeded expectations, and many go unresolved within required timeframes. These data demonstrate that the arbitration process is more costly and litigious than anticipated.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
The One Big Beautiful Bill’s looming impact on healthcare reimbursement has been well-documented, but there are plenty of other significant implications for hospital and health system operations.
Rethinking the healthcare workforce in the wake of OBBB explores the law’s potential impact on the healthcare workforce, as providers are already grappling with physician and nursing shortages. The article also outlines how providers can leverage technology and team-based care to forge a sustainable path forward, turning disruption into an opportunity to redesign workforce models.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
Medical supply company Medline is reportedly planning a big initial public offering next month. We get this story and more healthcare business and policy news on Monday.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Best regards,
The Gist Weekly team at Kaufman Hall








