In the News
What happened in healthcare recently—and what we think about it.
- CMS opens applications for $50 billion rural health fund. The Centers for Medicare & Medicaid Services (CMS) on Monday opened applications for the new 5-year, $50 billion Rural Health Transformation Program. Under the program, which was created under President Trump’s One Big Beautiful Bill (OBBB), CMS will distribute the money in $10 billion increments each year from 2026 to 2030. States must submit a one-time transformation plan by Nov. 5 detailing how they will use the funds to improve access, prevention, workforce and technology. Half of the funds will be divided equally among states that qualify, while the other half will be distributed at CMS’s discretion. CMS said that providers receiving funding need not be located in rural areas, so long as the money supports rural healthcare.
- The Gist: Rural healthcare funding has been a longstanding problem, with recent rural hospital and clinic closures underscoring the challenges they face. The Rural Health Transformation Program, as one of the largest federal investments in rural health in decades, may be a fix; but states are not required to channel funds directly to hospitals. Providers face the prospect of funding cuts on many fronts, including OBBB-related Medicaid funding changes and the failure to extend Affordable Care Act premium tax credits. This new program is not intended to offset those losses, but rather to enhance rural healthcare infrastructure in areas important to the Trump Administration. Funding will depend on how aggressively state governments engage, so hospitals should act now to shape their states’ applications. The ongoing ambiguity makes the implications of this program for rural hospitals significant but uncertain.
- Accreditation, CPT coding come to health AI. Artificial intelligence (AI) in healthcare is building institutional scaffolding to move into everyday practice. URAC, an independent accrediting body formerly known as the Utilization Review Accreditation Commission, on Monday unveiled the first accreditation program for health AI. The program is aimed at both developers and end-users, setting requirements around risk management, bias mitigation, transparency, data protection and monitoring. This comes after the American Medical Association last week released 288 new CPT codes for 2026 that carve out reimbursement pathways for AI-enabled services such as the use of AI-enabled systems to assess the severity of burn wounds. The Consumer Technology Association is adding another layer with its new standard for predictive AI, which emphasizes validation, accuracy and explainability.
- The Gist: These efforts are converging to give AI in healthcare the same infrastructure of oversight and reimbursement pathways on which established technologies rely. Slowly, healthcare AI is starting to build the sort of institutional trust it needs to move beyond pilot projects and vendor hype. Accreditation helps identify reputable vendors by creating a seal of approval that hospitals, payers and regulators can trust, while CPT codes unlock revenue streams that allow physicians and health systems to adopt these tools without eating the cost. Technical standards, meanwhile, put developers on notice that accuracy and fairness aren’t optional if they want market access. Taken together, these developments are early signs of AI’s maturation in healthcare—the unexciting but essential foundation that turns a promising technology into a mainstream tool of medicine. It’s less about dazzling capabilities and more about credibility, accountability and payment, which ultimately will drive adoption.
- 1 in 6 U.S. parents skip or delay vaccines for their kids: poll. Approximately 16% of parents in the United States have skipped or delayed a recommended vaccine for their children other than coronavirus or flu, a new poll has found. This includes 9% who have avoided the measles/mumps/rubella vaccine and 7% who have avoided the polio vaccine. The Washington Post/KFF poll, published Monday, found concerns about safety and side effects outweighed perceived potential benefit with a sizable minority of parents. The poll also found that trust in federal health agencies is weak, with fewer than half of parents confident in the Centers for Disease Control and Prevention (CDC) or the Food and Drug Administration to ensure vaccine safety. Even so, a large majority of parents support public schools’ requirement that students get measles and polio vaccines—even as Florida’s surgeon general has moved to “end all vaccine mandates” in the Sunshine State.
- The Gist: The poll comes as a new investigation finds widespread declines in childhood vaccination rates nationwide—a finding CDC data confirm. More counties are below the thresholds needed for herd immunity; the trend points to a higher likelihood of localized outbreaks of measles, pertussis and other vaccine-preventable illnesses that can quickly escalate into regional crises, as happened earlier this year in Texas. The poll also comes as former CDC director Susan Monarez testified Wednesday to a Senate committee that changes to the childhood vaccine schedule are imminent; meanwhile, the CDC’s Advisory Committee on Immunization Practices, which makes recommendations about who should receive vaccines, met this week under a cloud of controversy. The poll underscores that vaccine skepticism is now pervasive, even mainstream—a new reality to which health providers everywhere will have to adapt. With a rising number of sources of medical misinformation easily amplified on social media, evidence-based public health messages are being drowned out. This puts pressure on health systems to equip clinicians with clear, evidence-based talking points, expand outreach through schools and community groups, and strengthen collaboration with public health agencies. Pediatricians remain among the few trusted messengers for parents, a resource on which hospitals will increasingly need to rely.
Plus—what we’ve been reading.
- Patients caught in the middle of hospital-insurer standoffs. Published last month by KFF Health News, this article describes how prolonged contract disputes between hospitals and insurers leave patients vulnerable. It tells the story of one Missouri couple who spent weeks navigating a bureaucratic maze after their local health system and insurer let their network agreement expire. The provider and insurer were so far apart during contract negotiations that the state Senate intervened, prompting a resolution. However, the 3-month impasse left 90,000 patients out of network, exposing many of them to higher costs and delayed care. While coverage was eventually restored, the experience left patients wondering why they are routinely caught in the middle of opaque, high-stakes negotiations over which they have no control.
- The Gist: Hospital-insurer disputes are never easy and are growing more visible, and more disruptive. As healthcare delivery and labor costs rise and federal budget cuts loom, contract disputes are not isolated incidents. Between mid-2021 and mid-2025, 18% of hospitals publicly disputed with insurers over contracts, and 8% went out of network, according to one expert. They are growing contentious, with patients suffering the consequences and left to manage the fallout. In consolidated markets, a breakdown can disrupt care across an entire region. Some hospitals are left with no choice but to demand more for the care they provide to their communities while patients wait in limbo; but payers face pressures too, creating the potential for acrimony that threatens patient care.
Graphic of the Week
A key insight illustrated in infographic form.
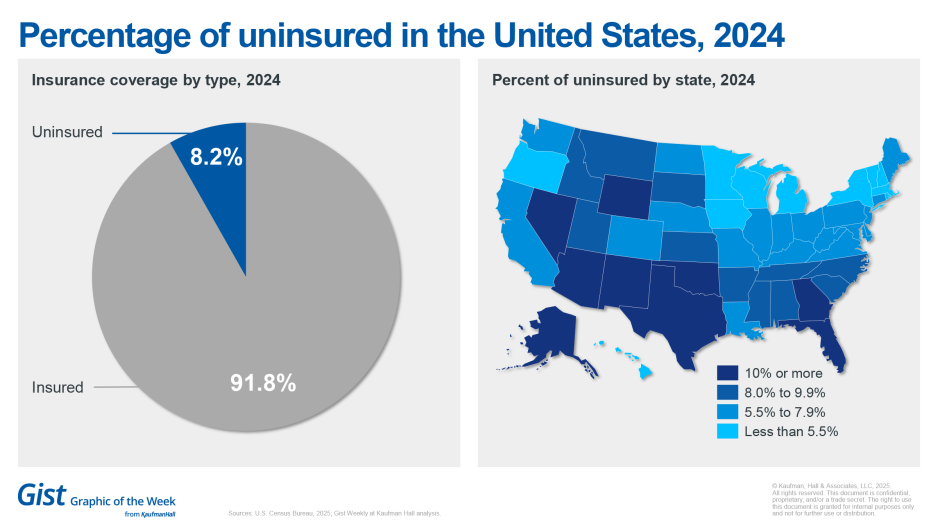
Uninsurance rates creeping up
Newly published data from the U.S. Census Bureau indicate that the rate of uninsurance in the United States is rising. The data, published this month, indicate that the national rate of uninsured hit 8.2% in 2024, up from 7.9% in 2023. The uninsured rate for all ages increased in 18 states and the District of Columbia and declined in two states from 2023 to 2024; for adults, it rose in 17 states and declined in 3 states between 2023 and 2024. Nine states currently have a total uninsured rate (including children) of over 10%. In 2024, the uninsured rate ranged from a low of 2.8% in Massachusetts to a high of 16.7% in Texas. The Census Bureau’s brief indicates that recent policy changes at the federal and state levels may have affected uninsured rates.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
For increasingly stretched-thin healthcare teams, ensuring consistent performance under stress is a difficult challenge.
The Framework for High Reliability Healthcare explores how organizations can transform how their teams think, act and lead—and embed safety, performance and resilience into the core of everyday operations.
On our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
HBO’s hit medical procedural The Pitt took home the Outstanding Drama Series trophy at this week’s Emmy Awards. On Monday, we hear an encore presentation of host J. Carlisle Larsen’s conversation with UPMC’s Sylvia Owusu-Ansah, M.D., about her experience serving as a medical consultant for the show.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Best regards,
The Gist Weekly team at Kaufman Hall








