In the News
What happened in healthcare recently—and what we think about it.
- ACA premiums set for spike. Affordable Care Act (ACA) marketplace premiums will jump by an average of 30% in 2026, according to a Washington Post analysis published last week. The increase, affecting approximately 17 million Americans who buy coverage through Healthcare.gov, would be the steepest annual rise since 2018, when benchmark plans climbed 37%. State-run marketplaces, which help provide coverage for an additional 7 million people, also report premium hikes, the analysis said. This follows reports from earlier this year that estimated a median rate hike of 18% among insurers, 11 points higher than last year, with many payers citing concern that healthy enrollees will drop coverage as premiums rise. The surge suggests the average family health plan will top $27,000 next year, up from $20,400 in 2024. This reflects higher medical utilization, rising hospital and drug costs, and the expiration of pandemic-era premium subsidies that had kept out-of-pocket costs low for many families.
- The Gist: A sharp jump in ACA premiums arrives at the worst possible moment for consumers and health systems alike. The government shutdown has left patients, providers and payers facing deep uncertainty. The combination of expiring subsidies, inflationary pressures and the government shutdown threatens to erode affordability. Meanwhile, 42 million Americans are threatened with the prospect of suspended Supplemental Nutrition Assistance Program benefits, which could drive more patients into emergency care. Hospitals should anticipate more uncompensated care and the potential for delayed treatment as patients may forego medical visits.
- CVS Health steps back from ambitious expansion. CVS Health on Wednesday announced it will close 16 Oak Street Health centers, about 7% of the network. The announcement comes less than two years after CVS Health acquired Oak Street Health, a network of primary care clinics focusing on seniors in underserved communities, for $10.6 billion. The closures come as CVS grapples with slower-than-expected growth and persistent cost pressures in its value-based primary care business. Oak Street Health, which serves Medicare Advantage patients through a capitated model, has been hit hard by higher utilization and rising expenses, forcing CVS to record a $5.7 billion impairment charge on the acquisition. CVS executives maintained that Oak Street Health’s mission remains central to CVS’s strategy to deliver integrated, community-based care.
- The Gist: The development demonstrates the difficulty in scaling risk-based models profitably while maintaining care quality and keeping costs under control, even for a company with CVS’s resources. Many systems have eyed similar models as a way to capture covered lives and diversify revenue streams beyond inpatient care. Yet while value-based primary care remains strategically attractive, it is operationally fragile. Oak Street Health’s experience shows the challenges associated with managing medical loss ratios and navigating Medicare Advantage risk arrangements. For health systems, the retrenchment offers a lesson about the economics of value-based primary care and the limits of retail-health consolidation. Health systems that plan to venture into retail health should temper expectations and stress-test their financial models with conservative assumptions. Achieving sustainable margins will likely depend on deep integration, disciplined expansion and an honest assessment of how much risk organizations can absorb.
- Appeal filed for lawsuit over use of the title “Doctor.” Plaintiffs this month appealed the dismissal of a lawsuit that challenges California’s restriction on use of the title “Doctor” in clinical settings. The lawsuit, filed by three nurse practitioners holding doctorates in nursing practice, challenged California’s 1937 law, which limited the honorific to licensed physicians within the context of a medical visit. The plaintiffs argued the restriction violated their First Amendment rights. The court, upholding the law as a reasonable regulation of commercial speech meant to protect consumers from misleading advertising, dismissed the lawsuit last month. It cited survey data showing that 39% of patients mistakenly believe that a nurse practitioner with a doctoral degree is equivalent to a physician. The American Medical Association and the California Medical Association called the ruling a win for patient safety and for “physician-led, team-based care.”
- The Gist: The ruling reinforces state authority to limit professional titles in healthcare advertising. It underscores an ongoing debate over “scope of practice” boundaries. By framing the issue around consumer protection and trust in advertising, the court signaled interest in clear language and professional title clarity for consumer understanding of the care they receive. The appeals court’s review could set precedent for how professional titles are regulated across other states. As APPs and other non-physician clinicians assume more prominent roles in the care delivery system, healthcare systems must also consider credential clarity and understanding.
Plus—what we’ve been reading.
- What good are doctors in an AI world? Published in September in The New Yorker, this article explores how advanced large-language-model tools are edging into diagnostic medicine and what this means for the traditional physician role. The article highlights how patients use AI chatbots to uncover missed diagnoses, examines experiments such as a face-off between an AI model and an expert doctor, and reviews research showing that AI can outperform clinicians in some controlled diagnostic scenarios. But it also stresses the dangers: AIs that hallucinate lab values, rely on incomplete data or steer patients away from care they actually need. It argues that the value of doctors won’t disappear, but their roles may pivot toward oversight, interpretation and care coordination.
- The Gist: Human judgment, context and trust still matter. Yet the technology curve is already creeping into clinical workflows, so remaining passive is not an option. Systems should start to define how AI tools will integrate with physicians and care teams as enablers that must be governed, audited and aligned with existing practices. This means investing in clinician training, reassuring clinicians that they are not being reduced to prompt-engineers detached from clinical judgment and ensuring governance around AI-driven advice. It also means maintaining the human touch so patients do not feel like data points in an algorithm. There is reason for cautious optimism, if the system can respect clinical reasoning and collaboration while steering through this technological evolution. Yet, doctors and patients alike are nervous and the “doctor-as-obsolete” narrative can threaten existing relationships if not controlled, so we must tread lightly.
Graphic of the Week
A key insight illustrated in infographic form.
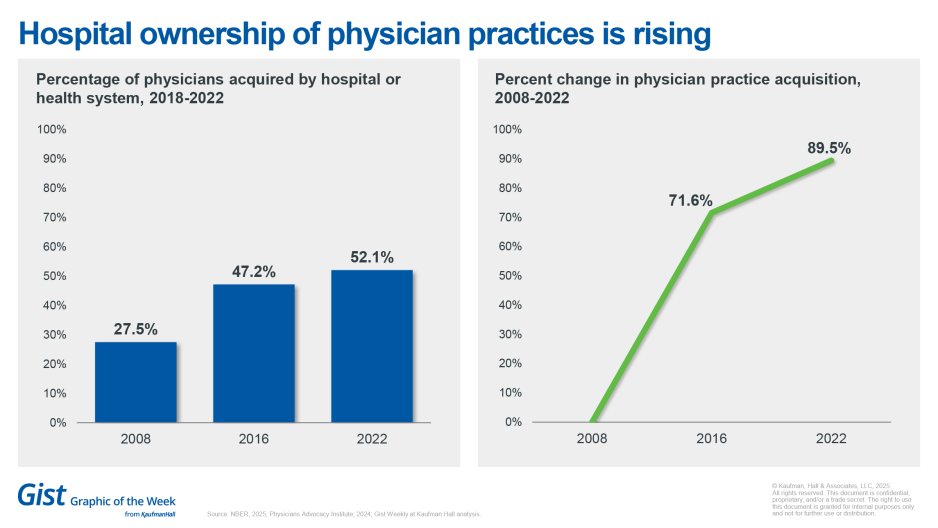
Hospital ownership of physician practices is rising.
Hospital ownership of physician practices has grown significantly from 2008 to 2022, new data show. A study from the National Bureau of Economic Research found that acquisition increased 89.5%, from 27.5% in 2008 to 52.1% in 2022. The growth was seen across all specialties, particularly for surgical specialties. From 2008 to 2016, acquisition increased for cardiologists, up 38.4% and general surgeons (28.1%), followed by moderate percent increases for primary care (18.1%) and OB/GYN (20.4%), economists found.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
When healthcare organizations apply their expertise, they can expect potential opposition from consumers, state and federal governments, and insurers.
Ken Kaufman’s latest blog considers the complicated evolution of expertise over the past 75 years. Today’s environment requires board and C-suite leaders to identify the basic principles of the organization about its role in medicine, patient care and public health and prepare to make decisions that remain true to these principles.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
The podcast is on hiatus on Monday, November 3. We will return with the latest healthcare business and policy news on Wednesday, November 5.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Best regards,
The Gist Weekly team at Kaufman Hall








