In the News
Before we get to the news… yes, we’re aware the federal government remains shut down. The Centers for Medicare & Medicaid Services announced Wednesday that most physician payments will not be held, reversing course from an earlier announcement. But with no signs of the shutdown nearing an end, we at the Gist Weekly must instead follow other stories. So…
What happened in healthcare recently—and what we think about it.
- Coalition for Health AI under fire as feds signal regulation is coming. In a column published in the Washington Examiner, Deputy Health and Human Services Secretary Jim O’Neill and Food and Drug Administration Commissioner Dr. Marty Makary sharply criticized the Coalition for Health AI (CHAI) for seeking to establish standards around health AI, accusing the 4-year-old trade group of stifling development and calling it “a virtual and unethical syndicate.” The criticism follows CHAI’s joint publication, co-authored by The Joint Commission, of voluntary guidelines on responsible use of health AI. CHAI, which includes major health systems, technology companies and academics, says it seeks to promote trustworthy AI in clinical settings. The column also comes just a few weeks after URAC, an independent accrediting body, unveiled the first voluntary accreditation program for health AI.
- The Gist: The exchange highlights ongoing debate over who should set the rules for AI in healthcare—industry or government. Traditionally, administrations from both parties have given private industry wide, but not unlimited, latitude to regulate itself, with a demonstrated willingness to step in when public health or safety is at stake. Only 18% of health systems report mature AI oversight, but federal officials complain that self-appointed groups backed by tech giants may prioritize private interests over public health and patient safety. Prominent legislators also are calling for regulation, particularly as states and local governments roll out a patchwork of rules that may complicate AI implementation and deployment. The European Union Artificial Intelligence Act offers a contrasting model, classifying AI according to its risk and placing most obligations on developers.
- New warning on the rise of antibiotic resistance. Common bacterial infections are becoming harder to treat, as resistance to widely used antibiotics continues to spread across the globe, the World Health Organization (WHO) warned this week. The WHO’s latest surveillance report highlights the challenge of antimicrobial resistance, finding that one in six infections tested in 2023 was resistant to standard antibiotics, with sharp increases since 2018 in several major bacteria linked to pneumonia, bloodstream infections and urinary tract infections. The report also highlights gaps in lab capacity and data reporting, especially in low- and middle-income countries where resistance is highest. WHO officials say the trend threatens decades of medical progress and urge countries to strengthen surveillance, invest in new treatments and curb unnecessary antibiotic use.
- The Gist: Antibiotics may be the single greatest healthcare success story of 20th century medical science, but that success is under threat. Bacteria are growing resistant to tried-and-true antibiotics, which many experts say are overused; but there simply aren’t enough new antibiotics in the pipeline to keep up. For hospitals, this is a red flag that routine empiric antibiotic protocols may not work for much longer. Rising resistance to core antibiotics means that standard treatment pathways risk becoming obsolete, pushing more cases toward expensive last-resort drugs or combination therapies. Hospitals will likely need to tighten diagnostics and ramp up their antimicrobial stewardship programs, ensuring antibiotic prescriptions are as precise as possible. Investments in point-of-care molecular tests, local resistance surveillance and antibiotic pipeline monitoring will become essential. And hospital administrators must prepare for increased costs, more complex case management and infection control burdens as treatment failures rise.
- Trump, AstraZeneca announce drug pricing deal. President Trump last week announced a deal with AstraZeneca, one of Europe’s largest drugmakers, to sell medications at “Most Favored Nation” levels, among other provisions. The agreement, heralded by both the White House and the drug company, follows the president’s May 12 executive order that encouraged the pharmaceutical industry to set U.S. prices equal to the lowest price available in peer countries and aimed to enable direct-to-consumer purchasing programs. The AstraZeneca announcement follows a similar declaration in late September from the White House and Pfizer that included limited information about TrumpRx, a new direct-to-consumer website where Americans will be able to buy medicine at discounted prices starting in early 2026.
- The Gist: Stubbornly high drug prices have long been a sore spot for U.S. consumers and providers alike. The AstraZeneca and Pfizer arrangements may lower some drug prices in certain circumstances, and any relief would be welcome. But details of the agreements have been kept confidential, which creates uncertainty for observers. The extent of the savings remains to be seen, as pricing through TrumpRx is not yet available and drugmakers already offer patient assistance programs for some of their medications. The trend of direct deals with pharmaceutical manufacturers bears watching as hospitals need to simultaneously improve care delivery through medication adherence and be aware of potential pricing changes.
Plus—what we’ve been reading.
- Wildfire smoke kills thousands annually. Published in September by NPR, this article details research from Nature that links wildfire smoke to approximately 40,000 premature deaths annually in the United States—a figure that could rise to 70,000 by 2050. The study integrates climate, fire and public health models to quantify how the increasing fire activity worsens people's smoke exposure and drives higher mortality from cardiovascular and respiratory conditions. The analysis shows that higher smoke exposure comes with health risks that linger for up to three years, leading to higher death rates. Researchers expect average smoke concentrations to double or even triple due to increased fire risk, and caution these risks may be underestimated—especially in heavily-populated urban areas where fires could release more hazardous pollutants.
- The Gist: Wildfire smoke has the makings of a potential chronic public health crisis. Wildfire smoke-related deaths often go unrecognized, obscured by underlying causes such as heart disease or COPD. The study reframes smoke from an episodic nuisance to a structural driver of long-term illness and death. For health systems, this marks a shift in which air quality is a health determinant with implications for cardiopulmonary and geriatric care and public health. The burden will be especially severe in wildfire-prone population centers where hospital closures may already strain access to care. Large, intensifying wildfires may further stress care delivery and the resilience of health infrastructure without adequate emergency preparedness.
Graphic of the Week
A key insight illustrated in infographic form.
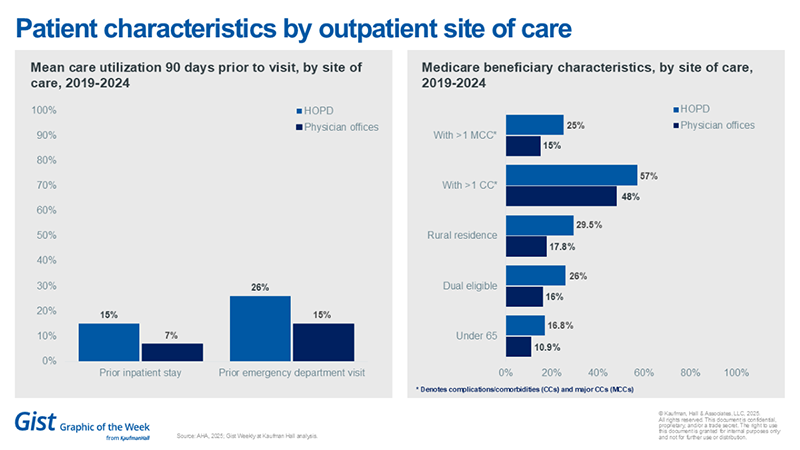
HOPDs treat sicker, more low-income and older patients: AHA study
A recent study published by the American Hospital Association found that hospital outpatient departments (HOPDs) care for more complex patients than independent physician offices. According to the study of Medicare beneficiaries who have visited an outpatient site of care between 2019-2024, patients who have visited an HOPD tend to be older and sicker than those visiting independent physician offices. They were also more likely to be from rural and lower-income areas, living with more severe chronic conditions and dually eligible for both Medicare and Medicaid. The study was prepared for the AHA by KNG Health Consulting. The findings suggest that site neutral payments may have an impact on patient access to care based on variations in demographics and utilization.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Integration isn’t just something that happens after a transaction. It ideally evolves every day through trust, alignment and shared purpose.
At the pace of trust—integration at every stage explores how leading health systems are rethinking integration as a continuous journey—one that strengthens culture, drives consistency and unlocks greater value across the enterprise.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
The next episode of the podcast will be Wednesday, Oct. 22. If you missed JC’s conversation with STAT News’s Lizzy Lawrence about pregnant women’s historical exclusion from clinical trials and the impact this exclusion is having today, give a listen here.
To stay up to date, tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Best regards,
The Gist Weekly team at Kaufman Hall








