In the News
What happened in healthcare recently—and what we think about it.
- Government shutdown ends; ACA subsidy vote will take place. The federal government reopened Thursday after President Trump signed a spending package, ending the 43-day shutdown that was the longest in U.S. history. The package will extend current government funding levels for certain programs and agencies through Jan. 30. The deal, a short-term continuing resolution and “minibus” of three full-year appropriations bills, did not extend Affordable Care Act enhanced tax credits, which are set to expire at the end of the calendar year and which Congressional Democrats had been pushing to extend. But with the deal, the Senate will consider extending the enhanced premium tax credits, with a vote promised by mid-December. Healthcare industry organizations called for lawmakers to extend the enhanced tax credits, which were initially established in 2021 (and extended in 2022) to expand ACA marketplace premium tax credits by boosting generosity and extending eligibility beyond 400% of the federal poverty level. The continuing resolution includes an extension of several key health programs and flexibilities (“extenders”) including the delay of Medicaid DSH payment cuts, extensions of the Medicare Dependent Hospital and Low Volume Adjustment programs, flexibilities around Medicare telehealth coverage, an extension of the Acute Hospital-Care-at-Home (AHCAH) waiver program, funding for Community Health Centers and a delay of statutory PAYGO (Pay-as-You-Go) requirements that would have caused future sequestration cuts to Medicare, among other policies.
- The Gist: Many view this deal as a policy win for President Trump and Congressional Republicans, who refused to negotiate the enhanced tax credits with the government closed. It may yet turn into a political victory for Democrats, who now have the opportunity to put Senators on the record as supporting or opposing the politically popular enhanced tax credits. The outcome is less clear in the House, which made no similar vote promise. It has been estimated that average premium payments for subsidized enrollees would rise by roughly $1,016 a year (an increase of about 114%) in 2026 compared with 2025 if the enhanced subsidy structure expires, although this would vary widely by state. Given President Trump’s suggestion to replace the tax credits with direct cash payments, it appears that Republicans recognize some degree of vulnerability on the issue. It’s too early to tell, but this may signal that elements of health reform could reemerge as a public policy debate for the first time since the failed attempt to repeal the ACA in 2017, in front of the 2026 midterm elections and perhaps into the 2028 election cycle.
- Moody’s declares stable outlook for hospitals next year. Moody’s Ratings gave the not-for-profit hospital sector a stable outlook in 2026 in its new outlook published Wednesday. The ratings service determined that the field’s gradual financial recovery is continuing, as operating cash flow margins inch up to roughly 6.5% to 7.0%, helped by tighter cost controls, steadier staffing and continued outpatient growth. The agency notes that most hospitals will sustain positive margin, though the pace of improvement has slowed and margins remain stuck below the pre-pandemic norm. Labor is a primary driver of cost challenges, given workforce shortages and rising compensation for certain specialty roles, including nursing, imaging, respiratory therapy and surgical support. It notes that federal and state efforts to control healthcare costs and improve care are creating financial uncertainty for hospitals, while cyber and environmental events present a growing operational risk. Moody’s said the outlook could change to positive if median operating cash flow margin exceeds 9% but could change to negative if it drops below 6%.
- The Gist: In this environment, stable is good. But this may be the calm before the storm. The One Big Beautiful Bill (OBBB) is projected to reduce cumulative federal health spending by approximately $1 trillion over the 10-year period ending FY2034, with the impact ramping up over time. This outlook is only for 2026; by 2027, as the financial effects of the OBBB begin to take hold, the skies could grow darker. Hospitals would be wise to use the coming year, with its stable outlook from Moody’s, to engage in sophisticated financial scenario planning to get out ahead of the OBBB’s changes before they hit.
- Canada loses measles elimination status. Canada has formally lost its measles elimination status after federal officials confirmed more than a year of uninterrupted transmission tied to a single strain circulating across multiple provinces, it was announced Monday. The Public Health Agency of Canada reported more than 5,000 cases this year in provinces across the country, with clusters in under-vaccinated communities and two infant deaths linked to the outbreak. Surveillance data showed declining two-dose MMR coverage in several regions along with delayed reporting, which made it harder to contain early spread. The determination by the Pan American Health Organization (PAHO) means Canada no longer meets the criteria for having endemic measles interrupted for at least 12 months. Venezuela lost its measles elimination status in 2018 and Brazil in 2019, but they both got it back after years of sustained public health efforts, PAHO officials said. Canadian health leaders say they plan to strengthen vaccine outreach, improve provincial and territorial coordination and rebuild confidence in routine vaccination.
- The Gist: Measles infections have hit their highest levels in the United States since the disease was declared eliminated here in 2000. The Canadian declaration demonstrates that vaccine hesitancy and its inevitable consequence of more infections are not confined to U.S. borders. Further, about two-thirds of Canadians live within 62 miles (100 kilometers) of the U.S. border, putting the problem right at our doorstep. The outbreak earlier this year in Texas and New Mexico has been tied to subsequent cases in South Carolina and Utah, although these ties are tenuous. But it’s clear that the United States’ elimination status is at risk. Hospitals should expect more suspected measles presentations, revisit staff vaccination policies and confirm rapid isolation procedures for rash-fever patients. Health systems also need to engage local public health agencies early, since delayed reporting is one of the factors that allowed the Canadian outbreak to take hold. Readiness only holds if vaccination, surveillance and frontline recognition stay tight.
Plus—what we’ve been reading.
- A ‘war’ on cancer science? Published in September in The New York Times, this article documents disruptions to grant processes at the National Cancer Institute. Review panels have been canceled and applications placed on hold, raising alarms among researchers about stalled progress. The article portrays a research community paralyzed by uncertainty, worried that funding decisions might depend on ideology. It also highlights the toll on morale among scientists who fear that decades of lifesaving work could be undone by shifting political winds.
- The Gist: When the United States launched its “war on cancer” more than 50 years ago, many hoped a cure would come quickly. Instead, progress came through decades of incremental breakthroughs. The five-year survival rate has risen from 49% in the 1970s to 68% today; it is estimated that every $326 that the federal government spends researching cancer extends a human life by one year, evidence that sustained public investment in research has saved millions of lives and built a world-leading scientific enterprise. That progress is now at risk. Funding delays mean fewer opportunities to collaborate on cutting-edge therapies and, in some cases, fewer lifesaving options for patients. The implications include challenges recruiting oncology investigators and diminished innovation pipelines. Health systems that depend on federal research dollars must reconsider their reliance on government grants, diversify support through philanthropy and industry, and build stronger internal capacity for innovation and evidence generation.
GRAPHIC OF THE WEEK
A key insight illustrated in infographic form.
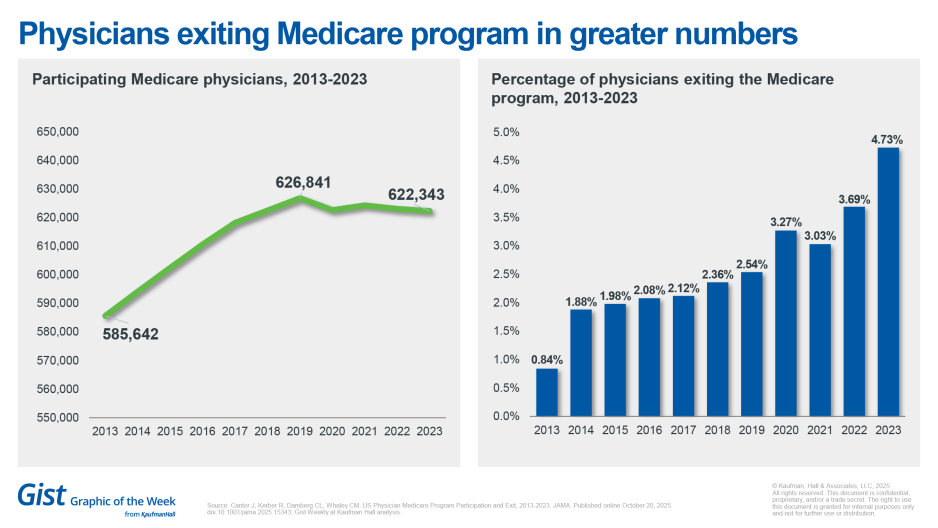
Docs exiting traditional Medicare in greater numbers
The number of physicians exiting traditional Medicare has accelerated, especially since the Covid-19 pandemic, with the annual exit rate climbing from less than 1% in 2013 to nearly 5% in 2023, a new JAMA study has found. The study, a review of Medicare fee-for-service claims data, found that while the total number of physicians in fee-for-service Medicare rose modestly over the decade, from about 586,000 to 622,000, departures have accelerated sharply in recent years. Participation peaked in 2019, then began a steady decline that has continued. Researchers found higher exit rates among older doctors, women, primary care physicians and those practicing in rural or underserved areas, but stopped short of making a claim about the impact of the pandemic. The trend raises concern that access to care for Medicare beneficiaries could erode even as the overall physician workforce grows; these patterns could exacerbate existing access gaps for older and rural Americans.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Artificial intelligence is rapidly reshaping healthcare, but the biggest challenge isn’t adopting the latest tools or standards — it’s about whether health systems are ready to deploy AI responsibly.
A new article explores how readiness — defined by strong governance, the ability to scale and alignment with enterprise priorities — is what separates meaningful innovation from costly experimentation.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
This past Monday, JC spoke with Chris DeRienzo, M.D., chief physician executive and senior vice president for the American Hospital Association. They discussed new data from Vizient and the American Hospital Association revealing that hospitals are seeing steady progress in surgical safety and survival. Complications such as severe bleeding and respiratory failure have declined significantly since 2019.
This coming Monday, the second part of the discussion turns to what comes after recent gains in surgical outcomes. Dr. DeRienzo talks more about the challenges hospitals face around post-acute care delays, workforce shortages, and the operational strain of caring for increasingly complex patients.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thanks for reading! The Gist Weekly will be on hiatus next week for meetings and the following week for Thanksgiving. We’ll be back on Friday, December 5. In the meantime, check out our Gist Weekly archive for past editions. We also have recent Graphics of the Week available here.
Best regards,
The Gist Weekly team at Kaufman Hall








