As 2025 came to a close, Congress could not come to a deal to extend Affordable Care Act (ACA) enhanced tax credits, which were first enacted during the Covid-19 pandemic and cut premium costs for millions of Americans. The deadline to extend those enhanced tax credits expired Dec. 31, 2025, and experts have warned that their expiration would result in significantly higher premiums and a loss of health insurance for millions. Late Thursday the House of Representatives voted 230-196 to extend the enhanced tax credits, but that bill appears unlikely to pass the Senate, where Senators are mulling their own ideas. Your Gist Weekly team is closely following this developing story. In the meantime…
In the News
What happened in healthcare lately—and what we think about it.
- ‘Superflu’ surges across the country. The year began with record-breaking flu activity across the United States, driven by a fast-spreading H3N2 variant that some observers have dubbed a “superflu.” The flu has been blamed for more than 5,000 deaths and 11 million illnesses already this season. The Centers for Disease Control and Prevention (CDC) reported that flu-related hospitalizations nearly doubled within a week to 19,000 (with 120,000 hospitalizations overall this flu season), with young children considered most vulnerable. The virus arrived earlier and more intensely than in past seasons, with “dramatic upticks” in respiratory cases across all age groups. The H3N2 subclade K mutation is contributing to the rapid spread, although experts say it hasn’t yet shown signs of increased severity. While the flu shot does not perfectly match this variant, experts say it reduces severe outcomes.
- The Gist: Hospitals are also managing simultaneous increases in RSV, Covid and norovirus, raising concerns about system capacity and co-infection risks. The flu is the first great stressor on hospitals in 2026, and it’s a doozy. It comes in a climate of rising vaccine hesitancy; as of late December, 42.5% of children in the United States had received a flu vaccination, down from 43.5% last season at this same time point. The CDC is no longer recommending routine pediatric seasonal flu vaccinations for all children 6 months and older in the United States, instead suggesting vaccine decisions should come via “shared clinical decision-making” between clinicians and parents. There is fear that the move will push pediatric flu vaccine rates even lower.
- Cervical cancer screening at home. The Department of Health and Human Services (HHS) this week published new screening guidelines for cervical cancer. The updated federal guidelines align with recent recommendations from the American Cancer Society and aim to boost screening rates, which have declined since 2021. HPV tests, which have usually been conducted in clinical settings will now be made available as an at-home, self-swab option for women ages 30 to 65 at average risk. HHS will require most private insurers to cover cervical cancer screening via self-collected samples. Experts hope the change will lead to more screening with increased flexibility and fewer cost barriers.
- The Gist: Approximately 13,000 cervical cancer cases are diagnosed annually in the United States, leading to 4,000 deaths a year, according to the latest CDC data. Expanded at-home cervical cancer screening follows other moves toward at-home diagnostics, such as flu and colon cancer tests. A series of isolated pilots has become a pattern: a shift toward screening models that favor accessibility and convenience over traditional encounters. Meanwhile, the healthcare field is reemphasizing screening in general, countering a movement from a decade ago that sought to reduce overscreening and what was perceived as unnecessary treatment that followed. Hospitals may need to guide this shift. Whether payment systems align to support hospitals’ role in patient education remains an open question.
- Utah to try AI for prescription renewals. The nation’s first state-approved program allowing AI to assist with prescription renewals was launched this week. Utah becomes the first state to try autonomous AI to participate in medical decision-making for prescription renewals for some chronic conditions with its announcement with Doctronic, an AI health platform. Under the pilot, residents can renew prescriptions for a $4 fee without talking to an actual prescriber. The service can process 30-, 60- or 90-day renewals for certain medications that have already been prescribed, but will not issue new prescriptions nor handle refills for controlled or addictive substances. The initiative aims to streamline medication access, specifically targeting noncompliance, a key driver of avoidable health costs.
- The Gist: It’s a grand experiment: Utah is pushing the boundaries of how far AI can go, unsupervised, in clinical decision-making. If it goes well, the Utah program could point a way toward easing administrative burden and improving medication adherence at scale. But there are the usual concerns: the tendency of chatbots to “hallucinate” falsehoods or encourage a user to act on bad information. Nevertheless, chatbots have quickly become a trusted resource; more than 40 million people use ChatGPT daily for health information. This pilot is narrower; it will track refill timeliness and adherence as well as patient access and satisfaction, workflow efficiency, cost impacts and safety outcomes. By regulating innovation in real time, Utah is creating a structured space for clinical-grade automation. The future of AI in healthcare appears to hinge on trust and policy design rather than technical capability—which happens to be a concern in our reading below.
Plus—what we’ve been reading.
- Physician, heal thy profession. Published in December in The New Yorker, this article considers how the traditional role of medical doctors as trusted experts has been upended, perhaps irreversibly. Whereas physicians once enjoyed a near monopoly on medical knowledge and treatment, they now compete with Internet and AI tools, direct-to-consumer services and wellness influencers for patients’ attention and trust. The author, himself a practicing physician, opens with the story of a patient who avoided doctors entirely until an AI alert sent him to the hospital; the anecdote illustrates a trend of patients relying on social media, fringe movements and digital diagnostics long before they visit a clinician. Trust in physicians has slid, and surveys (e.g., Gallup) show many people think online sources or “self-research” can match a physician’s expertise. Faced with these pressures, the author argues, doctors must stop considering themselves as gatekeepers and reassert their value as healers through empathy, communication, and collaboration rather than cultural authority.
- The Gist: For hospitals, this is a wake-up call about how patients want to interact with clinical providers. Health systems that cling to old models of authority risk losing relevance and patient engagement as more people turn to digital tools for first-line advice. Social media and the Make America Healthy Again movement are only the latest developments in the paradigm shift, demonstrating patients’ demand for agency. The piece underscores a growing need for hospitals to integrate technology thoughtfully and position clinicians as accessible interpreters of complex information. In practice, that means investing in care models that meet patients where they already are (e.g., online triage, digital communication channels) and proving that hospitals remain a necessary part of the care journey in a landscape crowded with alternatives. The good news: “even today, in a moment of pitched cynicism… Americans of all backgrounds and politics still overwhelmingly trust their own doctors.”
Graphic of the Week
A key insight illustrated in infographic form.
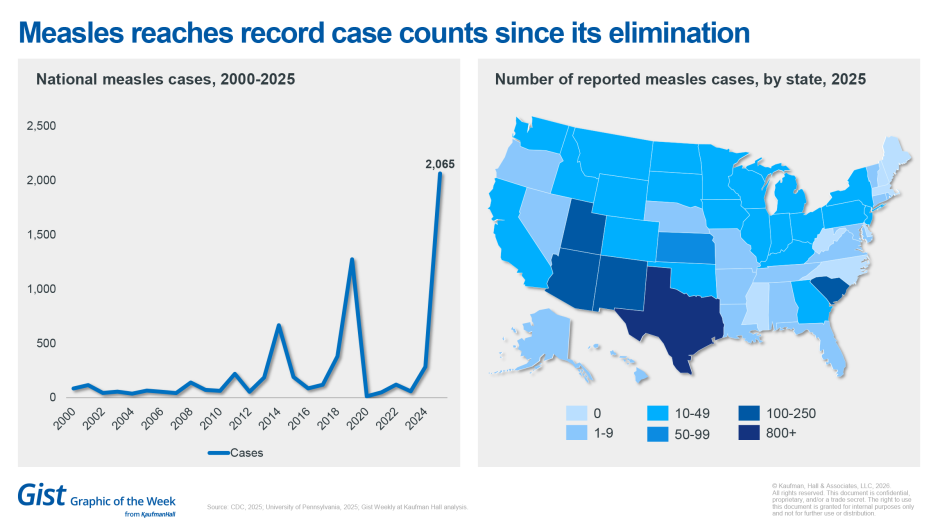
Measles reaches record case counts since its elimination
Last year, the United States experienced its worst measles outbreak in more than three decades, with more than 2,000 confirmed cases reported by the CDC across 49 outbreaks nationwide. Approximately 93% of cases occurred among unvaccinated individuals. As measles cases continue to rise, a national survey conducted in November and December by the Annenberg Public Policy Center of the University of Pennsylvania found a small but statistically significant decline in the proportion of Americans who would recommend the measles/mumps/rubella (MMR) vaccine to someone in their household. The survey also identified diminished public perceptions of the safety and effectiveness of the MMR vaccine, as well as vaccines for seasonal flu and Covid-19. Despite these declines, the public continues to view vaccination as the most effective defense against diseases like measles. About 11% of patients are still being hospitalized for measles, so hospitals may need to be ready to employ isolation precautions to prevent in-hospital spread. Measles was officially eliminated in the United States in 2000, which means the country had not seen large outbreaks and had not had 12 months or more of uncontrolled domestic transmission of the virus; but that status now appears to be in question.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
In an era of increasing financial pressure, reducing non-labor expenses requires a coordinated, strategic approach—blending analytics, process improvement and cross-functional collaboration.
Explore the framework that helped one health system unlock savings while strengthening supplier relationships and clinical alignment.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
The podcast is catching up on healthcare business and policy news after a busy end to the year. On Wednesday, OpenAI announces a new ChatGPT Health tool it's releasing. We get that story and more.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thank you for reading! Please stay tuned for next week and check out our Gist Weekly archive for past editions. We also have our recent Graphics of the Week available here.
The Gist Weekly team at Kaufman Hall








