In the News
The biggest news of the week—and what we think about it.
- MA rate proposal sends shockwaves across the market. Medicare Advantage (MA) payments to health plans would rise just 0.09% in 2027 under the advance notice of methodological changes for MA capitation rates and Part C and Part D payment policies (“Advance Notice”) that was published this week. The increase in payment, proposed by the Centers for Medicare & Medicaid Services (CMS), would be well below this year's 06% update. In addition to other proposals, CMS plans to reform how risk scores are calculated by excluding all diagnosis codes not directly linked to a previous medical encounter. This adjustment accounted for a 1.53 percentage point reduction to year-over-year payments, if finalized for 2027. CMS says this proposed reform would improve program integrity, but health plans that rely on these diagnoses may lose significant revenue. Shares of major Medicare Advantage insurers plummeted as insurance industry representatives warned the proposals in the Advance Notice could lead to benefit cuts and higher costs for enrollees.
- The Gist: The market reaction suggests health insurers have reason to worry, which could have downstream consequences for hospitals. The proposal tightens risk adjustment rules to curb upcoding, which has inflated MA reimbursements—an issue federal investigators have flagged. Insurers may respond by cutting benefits, shifting costs to employers and patients and possibly taking a harder line on provider price negotiations. The comment period runs through Feb. 25, with a final rate announcement due by April 6, so these policies may change.
- Rural health leaders await funding uncertainty. Rural health leaders this month expressed uncertainty about Rural Health Transformation Program funding. As states raced to submit their applications for the new federal program, which was created under President Trump’s One Big Beautiful Bill, hospital executives said their recommendations went unheard and that the program may leave hospitals underfunded as they face rising financial strains. Although allocations for states were announced last December, including baseline awards and additional funding based on rurality and technical needs, states were resubmitting budgets this week. According to the Notice of Award timeline, funding might not reach states until March.
- The Gist: Rural Health Transformation Program funding was never guaranteed to provider organizations. Rural health providers have cause for concern as funding may get wrapped up in state initiatives. Early state application documents suggest that some states will prioritize workforce development, technology implementation and competitive grants for community partnerships. Rural providers should prepare for collaborations to strengthen health delivery rather than anticipate funding to mitigate operating losses. Community partnerships focused on regional or state-level priorities may be the name of the game, especially for struggling facilities.
- Serious reportable events reporting to streamline. The Joint Commission and the National Quality Forum (NQF) on Monday announced a move to align their patient safety reporting frameworks. The Joint Commission will adopt NQF’s updated Serious Reportable Events (SRE) List as its own Sentinel Events List starting next January while retaining three workforce safety events from its legacy list, the organizations said in a news release. The alignment eliminates parallel lists and is intended to reduce redundancy and confusion in safety event reporting. To help healthcare organizations transition their SRE reporting, the organizations are providing technical support and have published a report with application guidance and a crosswalk of events. The change stems from The Joint Commission’s 2023 affiliation with NQF, in which the two organizations pledged to reduce the reporting burden by aligning common frameworks.
- The Gist: NQF introduced its list of SREs—informally known as “never events,” because they should never occur—in 2002. They include incidents like wrong-site surgery or patient death or serious injury associated with the use of contaminated drugs or devices. More than 30 states and hundreds of healthcare organizations use the since-updated SRE List for required or voluntary reporting, although many do so with modifications, making cross-system comparison difficult. This alignment constitutes an overhaul of how safety events are defined, tracked and reported under accreditation and quality programs. The separate Sentinel Events and SRE List together have comprised a data collection and reporting burden; the alignment should simplify compliance. Ideally, the unified list and guidance should support more reliable benchmarking and trend analysis, helping systems pinpoint risk patterns and prioritize preventive action. Hospitals should familiarize themselves with the SRE list now, updating internal protocols and educating staff on the changes, so they are ready for implementation and can maintain accreditation without disruption.
And—what we’ve been following.
- The South Carolina measles outbreak is now larger than last year’s Texas-based outbreak. This comes as the United Kingdom and other European countries lose their elimination status.
- The number of heart disease and stroke deaths has declined, according to a recent study from The American Heart Association.
- Approximately 30,000 Kaiser Permanente healthcare workers in California and Hawaii began an open-ended strike this week.
Plus—what we’ve been reading.
- For older Americans, the caregiving challenge. Published earlier this month in The Washington Post, this article examines the challenges of elderly spousal caregiving. As lifespans increase and family sizes shrink, a growing share of seniors in their 60s, 70s and beyond are assuming around-the-clock care for partners with chronic conditions like dementia. Nearly half of spousal caregivers are 75 or older themselves who must juggle duties such as bathing, dressing and incontinence care while coping with social isolation and their own health issues. With fewer adult children nearby to step in, these seniors can burn through savings paying for in-home help or long-term care and risk injury from the physical strain of caregiving. Experts say this “locked in” caregiving is more difficult than the way adult children tend to aging parents, with deeper emotional tolls and little relief. The trend reflects broader caregiving shifts in the United States, as roughly one in four adults now provides uncompensated care to a loved one.
- The Gist: The rising tide of spousal caregiving has immediate operational and strategic implications for hospitals. Health systems see firsthand the downstream effects of unpaid caregiver strain: delayed discharges when home support is inadequate, higher readmissions linked to inconsistent care at home and greater demand for post-acute and respite services. Hospitals will need to invest more in caregiver education and discharge planning that accounts for the capability and limitations of older spousal caregivers, not just adult children. There is also a growing case for stronger partnerships with community-based organizations to extend support beyond the hospital walls, whether in training, home assessments or transitions to home health, ensuring appropriate, high-quality care. Policymakers are increasingly considering how to support family caregivers because they are, in effect, an extension of the long-term care system. Ignoring their needs would amplify pressure on acute care settings ill-prepared for a population aging in place without professional support.
Graphic of the Week
A key insight illustrated in infographic form.
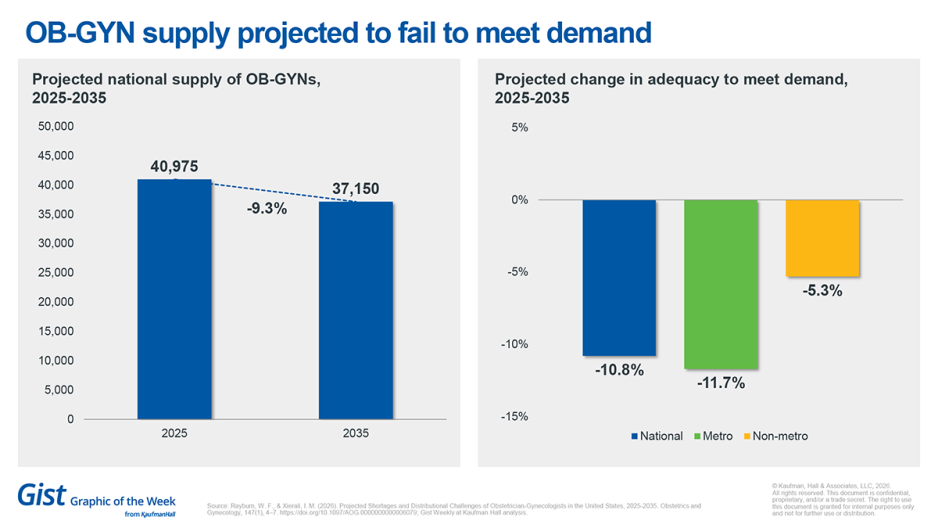
OB-GYNs in short supply
A recent study published in Obstetrics & Gynecology projects a worsening mismatch between obstetrician-gynecologist (OB-GYN) supply and patient demand over the next decade. Nationally, the OB-GYN workforce is 93.4% adequate to meet current demand, and total supply is projected to decline by 9.3% by 2035. As a result, adequacy is expected drop 10.8 percentage points nationally, with sharp differences in metropolitan and non-metropolitan areas. Geographic variation is pronounced at the state level, underscoring the uneven distribution of access across the country. In the face of this trend, hospitals may need to reassess how obstetric care is delivered in their communities. This includes understanding local demand for OB-GYN services, the prevalence of high-risk obstetrics and the proportion of the population whose needs could be safely met by other clinical providers. In some cases, health systems may need to reconsider whether they should retain their OB-GYN service lines at all.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Can your emergency department (ED) afford to stay average?
A new article explores why average ED performance isn‘t safe or sustainable—and how underperformance in EDs affects patient safety, financial margins and staff morale. Learn what high-performing systems are doing differently to address the challenge.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
Last Monday’s episode explores the conundrum that while health systems are adding more advanced practice providers (APPs), many organizations aren’t seeing the payoff. Kaufman Hall’s Bonnie Proulx joins JC to unpack why physician/APP models often fall short, and what leaders can do to make team-based care work.
Physicians face higher rates of depression, anxiety and suicide risk than the general population, yet a large proportion never seek mental healthcare. In this upcoming Monday’s episode, Jesse Ehrenfeld, M.D., discusses newly published JAMA research that looks at why doctors are so hesitant to get help, from medical culture and stigma to concerns about confidentiality and professional consequences; and what may finally be starting to change.
Thank you for reading! Please stay tuned for next week and check out our Gist Weekly archive for past editions. We also have our recent Graphics of the Week available here.
The Gist Weekly team at Kaufman Hall