In the News
The biggest news of the week—and what we think about it.
- Overdoses decline across the United States. Drug overdoses have declined significantly in the past year, according to new data published Wednesday by the Centers for Disease Control and Prevention (CDC). The CDC found a 20.6% decline in overdoses. While the monthly toll has not yet returned to pre-pandemic levels, the decline has been the biggest drop in decades, analysts say. The data are provisional but suggest that almost all states have had declines. The findings reflect a sharp reversal after overdose deaths started climbing in the 1990s with overdoses involving opioid painkillers, followed by deaths from heroin and fentanyl.
- The Gist: The decline is welcome news, full stop. The cause could come from a number of factors. Some analysts suggest it may be due to China’s crackdown on fentanyl supply and its chemical components. But the explanation is likely more complex. Changes in opioid prescribing practices, naloxone availability and treatment breakthroughs have likely contributed to the decline. But new addictive substances, like medetomidine overdose cases that began in Philadelphia in 2024 (which burdened emergency departments with more than 7,000 withdrawal cases in 2025) threaten the trend. For hospitals, the overdose decline is to be celebrated but should also provide a moment to prepare to meet the needs of substance use patients if the drug use epidemic changes shape.
- Congressional leaders agree on health deal. A bipartisan group of leaders from both houses of Congress reached agreement this week on a healthcare package, commonly referred to as “extenders.” The compromise, part of a broader deal to fund four of the remaining federal agencies (known as a “minibus”) before the end of September, would extend Medicare telehealth coverage through Dec. 31, 2027 and the Acute Care Hospital at Home Program through Sept. 30, 2030. It would also eliminate $16 billion in Medicaid Disproportionate Share Hospital payment reductions slated to take effect in the 2026 and 2027 fiscal years and reauthorize programs such as the Dr. Lorna Breen Health Care Provider Protection Act through FY2030.
- The Gist: The agreement appears to be a standard extension package. It could pass before the end of the month, although it hinges on passage of the minibus, which may still have some Republican opposition. Nevertheless, the agreement is notable for what it does not contain: an extension of the enhanced advance premium tax credits, which expired at the end of 2025. These enhanced tax credits are popular, and their expiration has led to sharp premium increases, but Congress has thus far been unable to reach a bipartisan agreement to extend them. Even so, the agreement does contain several measures that hospitals will appreciate by extending several other Medicare payment programs.
And—what we’ve been following.
- The measles epidemic continues to surge, with reports of an outbreak in South Carolina bringing the case total to 646.
- Approximately 31,000 registered nurses and health professionals from the United Nurses Associations of California/Union of Health Care Professionals issued a 10-day strike notice to Kaiser Permanente this week. They are expected to picket at more than 220 healthcare sites starting Jan. 26.
- UnitedHealth Group announced that it will rebate profits from its Affordable Care Act marketplace health plan selections to consumers in 2026
- The United States is finalizing its exit from the World Health Organization this week, a year after President Trump issued an executive order announcing the withdrawal.
Plus—what we’ve been reading.
- New ‘smart pill’ could change adherence tracking. Published earlier this month in the academic journal Nature, this article shares the development of a biodegradable “smart pill” that can confirm when a patient swallows a medication. The capsule contains a tiny RFID tag wrapped in a coating that dissolves in the stomach, triggering a wireless signal that confirms ingestion. Unlike earlier digital pills, most of the materials safely break down in the body, reducing safety concerns and electronic waste. Tests in animals showed the system worked reliably and fully degraded after use. The study may point to a more practical way to measure medication adherence, which remains a major and costly problem in healthcare.
- The Gist: This kind of technology could have major implications for how clinical providers monitor medication adherence after discharge. Instead of guessing based on refill data or patient self-report, care teams might know when doses are missed and intervene earlier. Ideally, this could help reduce readmissions, complications and treatment failures, especially for high-risk therapies like transplant drugs. More reliable adherence data could also support better care coordination and more targeted patient outreach. However, it is unclear whether patients might accept the new technology. In addition to patients’ response, cost and reimbursement are still concerns to be resolved. But the concept is attractive: fewer missed doses should lead to fewer downstream problems.
Graphic of the Week
A key insight illustrated in infographic form.
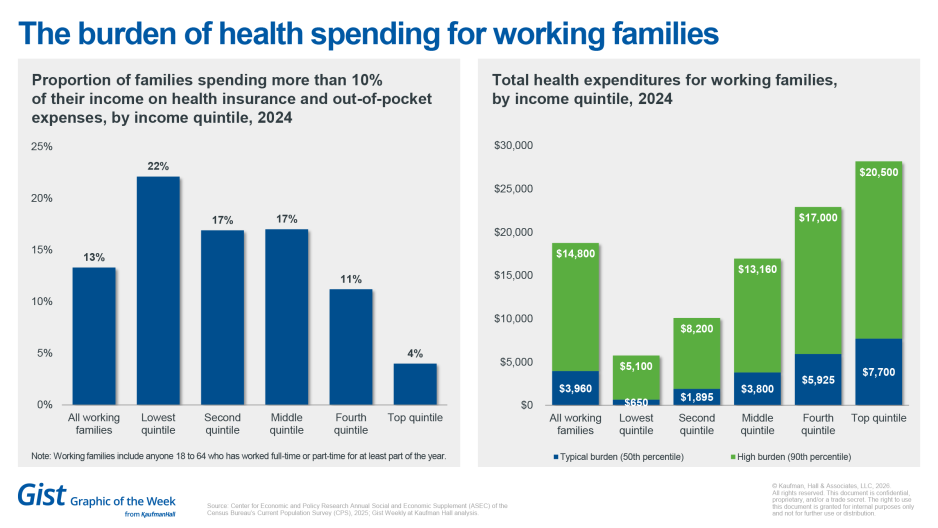
The burden of health spending for working families
As healthcare inflation continues to outpace overall inflation, American families are spending more on care and bearing that cost unevenly. A recent analysis from the Center for Economic Policy and Research found that the typical working family spent about $3,960 to $14,800 on healthcare. Although healthcare spending rises with income in absolute dollars, reflecting factors such as family size, the relative cost burden tells a different story. Workers in lower-income families were more likely to spend more than 10 percent of their income on healthcare than those in the highest income quintiles, even as higher-income families spent more in total dollars.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Health systems are running out of financial runway, as challenges including cost pressures, workforce shortages, regulatory upheaval and high patient expectations continue to pile up.
The next few years will determine which organizations pull ahead and which fall permanently behind — and 2026 will shape that trajectory.
Two new Vizient reports explore the key trends resetting healthcare’s financial foundation – and the steps leaders can take to keep their organizations ahead of the curve:
- New margin math: Healthcare industry outlook 2026 | Vizient
- Get ready for a reset: Healthcare strategy playbook 2026 | Vizient
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
This Monday, health systems are adding more advanced practice providers (APPs), but many systems are not seeing the financial payoff. Kaufman Hall’s Bonnie Proulx joins JC to unpack why physician/APP models often fall short, and what system leaders can do to make team-based care work.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thank you for reading! Please stay tuned for next week and check out our Gist Weekly archive for past editions. We also have our recent Graphics of the Week available here.
The Gist Weekly team at Kaufman Hall








