In the News
What happened in healthcare recently—and what we think about it.
- Hospitals improve patient safety, new report finds. Hospitals made substantial, sustained gains in patient safety and outcomes from late 2019 through mid-2025, even as they cared for a larger and sicker patient population, according to an analysis released last week by the American Hospital Association and Vizient®. The analysis, based on data from Vizient Clinical Data Base, found that patients hospitalized in the second quarter of 2025 were nearly 30% more likely to survive compared with pre-pandemic baselines, resulting in an estimated 300,000 additional lives saved between April 2024 and March 2025. Hospitals treated 4% more patients with 5% higher acuity yet significantly reduced central line-associated bloodstream infections by 24% and catheter-associated urinary tract infections by 25%. Preventive breast and colorectal cancer screenings rose 95% over the same period, reflecting expanded outreach and earlier detection efforts.
- The Gist: This report provides encouraging evidence that hospitals are making real progress in patient safety. Hospital leaders credit data-driven safety initiatives, advanced analytics and collaborative benchmarking programs for driving these improvements, saying the results underscore the impact of continuous quality improvement at a moment when patient complexity and operational pressures remain high. These trends signal that sustained focus on patient safety is yielding tangible results, offering a positive outlook for the quality of care and demonstrating that ongoing investment in infrastructure and preventive strategies can meaningfully improve outcomes.
- OPPS final rule expands site neutral. The Centers for Medicare & Medicaid Services (CMS) finalized wide-ranging updates to its outpatient prospective payment system (OPPS) late last month, setting the stage for reimbursement and reporting changes in 2026. The final rule expands CMS’s site-neutral payment policy to include drug administration services in excepted off-campus provider-based departments and provides a phased elimination of the inpatient-only list. The agency set a 2.6% increase for the outpatient department schedule for hospitals that meet quality reporting requirements, slightly higher than was proposed earlier this year. CMS is also updating the methodology for Overall Hospital Quality Star Ratings and adding new price transparency obligations. Most changes take effect Jan. 1, 2026, while enforcement of transparency rules begins later to allow additional time for compliance. The new payment policies affect approximately 4,000 hospitals and 6,000 ambulatory surgery centers.
- The Gist: For hospitals, the rate update offers modest relief but not enough to ease broader margin pressures. The site-neutral expansion was not unexpected and is likely to continue, as CMS earlier signaled through solicited comments that additional site-neutral payment policies remain on its radar. The elimination of the inpatient-only list will likely push more procedures into outpatient settings. This could significantly impact revenue streams for health systems, especially those with large hospital-based outpatient volumes. Health systems that haven’t already started impact assessments and strategic planning to mitigate risk should do so as soon as possible. They also need to tighten their data operations as CMS revamps star ratings and requires market-based reporting tied to future rate setting. Although CMS postponed enforcement of new price transparency requirements until April, that delay is short for health systems that may still be scrambling to comply.
- HHS unveils AI strategy. The Department of Health and Human Services (HHS) last week introduced a strategy to expand the use of artificial intelligence across its agencies. The strategy includes shared AI infrastructure, new workforce training initiatives, stronger research standards and AI tools to modernize care and public health. The rollout comes amid an intensifying national fight over AI regulation. Deputy Secretary Jim O’Neill recently sidestepped questions about a proposal backed by President Trump to preempt state AI laws with a single federal “rulebook.” Critics warn that removing state protections could heighten risks like deepfake AI abuse and AI-enabled cyber threats on Affordable Care Act health exchanges.
- The Gist: HHS’s AI strategy, dubbed “OneHHS,” arrives at a time when regulatory uncertainty may limit innovation just as AI’s clinical potential accelerates. Health systems struggle to navigate a patchwork of state rules and laws that make it difficult to scale AI-enabled services across state lines. While a national strategy raises concerns about patient safety and data protections, clearer federal guidance—or a coordinated national framework—would provide consistency to deploy AI at scale. In this sense, HHS’s push to articulate a unified strategy could be a constructive first step: not a substitute for robust safeguards, but a signal that federal leadership may help align a fragmented regulatory landscape.
Plus—what we’ve been reading.
- Advanced prostate cancer diagnoses rise. Published in September by The New York Times, this article reveals that prostate cancer diagnoses are increasingly being made at later, less treatable stages. A report from the American Cancer Society links this to a 2012 recommendation by the U.S. Preventive Services Task Force that discouraged routine PSA screening in healthy men. The guidance, now in process of being updated, aimed to reduce overtreatment of less aggressive cancers but may have led to under-detection of aggressive disease. But since 2014, late-stage cancers have been climbing up to 4.8% per year. The study also finds persistent racial disparities, with Black men facing both higher prostate cancer and death rates.
- The Gist: Experts continue to debate the right balance between screening harms and benefits, especially as life expectancy increases and imaging technology improves. A well-intentioned pullback on routine PSA screening may have contributed to a rise in late-stage prostate cancer, particularly among older men. The effects took years to surface—illustrating how changes in screening policy can echo across years of clinical outcomes. The result: more diagnoses when disease is metastatic and less treatable. The shift exposes tensions in screening and highlights a need to reconsider recommendations for aging populations. As the Task Force updates its guidelines, health systems may face renewed pressure to align screening practices with evolving longevity and risk patterns.
Graphic of the Week
A key insight illustrated in infographic form.
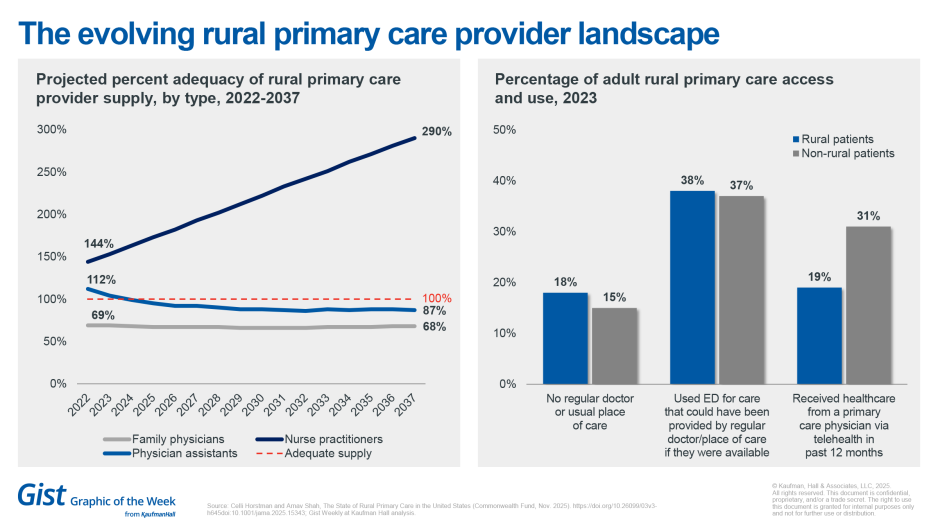
The evolving rural primary care provider landscape
Newly published projections from The Commonwealth Fund highlight persistent physician shortages, limited telehealth access and infrastructure and payment challenges in rural healthcare. The projections were published in The State of Rural Primary Care in the United States and drawn from the Commonwealth Fund 2023 International Health Policy Survey and federal health workforce data. They find that rural communities already have fewer physicians than they need, a shortage that is expected to continue. To fill the gap, The Commonwealth Fund projects that rural communities will increasingly rely on advanced practice providers (APPs), who are already more abundant. While overall rural healthcare workforce availability may be sufficient when APPs are included, disparities remain in telehealth access. Limited access to physicians and telehealth has also contributed to higher use of emergency departments and other costly sites, a trend exacerbated by rural hospital closures and greater transportation needs.
This Week at Kaufman Hall
What our experts are saying about key issues in healthcare.
Health systems faced significant challenges in 2025 that will likely continue into 2026, from managing non-labor expenses to strengthening the workforce, expanding access, and navigating payer reimbursement.
Kaufman Hall’s 2025 Performance Improvement Outlook highlights the key challenges shaping executive priorities, while also outlining the actions health systems are taking to navigate disruption and build long-term resilience.
On Our Podcast
The Gist Healthcare Podcast—all the headlines in healthcare policy, business and more, in 10 minutes or less every other weekday morning.
Last Monday, Kristine Lee, M.D., Associate Executive Director of Virtual Medicine, Technology, and Innovation at The Permanente Medical Group, joined host J. Carlisle Larsen to discuss its year-long pilot that tested an ambient AI scribe and its impact on physician burnout.
This Monday, Michael McAuliff of Modern Healthcare joins us to review the federal healthcare policy changes we saw this year, regulations we ultimately did not see in 2025 and what could be in store for 2026.
To stay up to date, be sure to tune in every Monday, Wednesday and Friday morning. Subscribe on Apple, Spotify, Google or wherever podcasts are available.
Thanks for reading! We’ll see you next Friday with a new edition. In the meantime, check out our Gist Weekly archive for past editions. We also have all of our recent Graphics of the Week available here.
Best regards,
The Gist Weekly team at Kaufman Hall








