
This is the first of a three-part Performance Improvement series. Future articles will explore reducing clinical variation and strategies for engaging physicians in performance improvement.
A New View of Performance Improvement
Hospital and health system leaders are currently facing multiple threats to the long-term financial stability of their institutions. As healthcare costs continue to rise, private insurers and the federal government are intensifying pressure around payments. A wave of new competitors, from physician-owned surgery centers to retail and virtual clinics, are increasingly offering services at far more affordable prices to consumers, unencumbered by the cost structure of legacy providers. In turn, these threats are forcing hospitals and health systems to determine how to pivot from the traditional delivery chassis to new capabilities in digital and retail healthcare.
The imperative for hospitals to embark on continuous, organization-wide cost reduction initiatives has never been greater. Unfortunately, many of the strategies that organizations once successfully used to manage costs no longer measure up to the challenge. All too often, cost reduction initiatives are stymied by factors including a lack of systemic accountability, a focus on isolated, project-based improvements, fatigue, and the lack of a clear measurement system for tracking savings. In some instances, poorly planned implementation can even damage organizations’ long-term financial performance, and many organizations struggle to sustain initial savings over time.
The recent proliferation of information from electronic health records (EHRs) poses another unique opportunity and challenge for cost reduction efforts. While EHRs offer vast amounts of data on clinical encounters, often in real-time, many organizations lack the ability to sift through the noise and analyze underlying trends—leading to information overload instead of meaningful insight.
Hospitals and health systems that intend to successfully transform their operations for a new era must start by identifying clear financial targets at the outset that ultimately support the long-term financial sustainability of the institution, and make a sustained commitment to continuous improvement.
Organizations must commit to an inclusive, team-based approach that engages the finance department, overarching operations, and the entire physician enterprise.Those best practices should be supported by robust comparative analytics that incorporate data on the quality and cost of care, the development of baseline targets for continuous improvement, and a staffing approach that employs state-of-the-art analytics to staff to demand. Finally, health systems must be able to make hard decisions about the long-term necessity and sustainability of their current facilities.
With the right infrastructure and systems in place, organizations can integrate their clinical and financial management and genuinely transform their organizational approach to managing costs. Ultimately, cost reduction should be part of an organization’s DNA – and a continuous journey, not a destination.
Pitfalls
- Lack of accountability (or structures and mechanisms to hold leaders responsible)
- Project mentality (“We do this during budget season”)
- Improvement fatigue
- No method for tracking sustainable savings
Best Practices
- Team effort between finance and operations
- Informed and engaged physician enterprise
- A structure for driving accountability and managing results
- A platform for managing program implementation
Setting and Sustaining Realistic Targets: A Data-Driven Approach
As hospital leaders confront the prospect of long-term, sustained declines in payment, the need to develop, establish, and communicate financial targets for cost reduction initiatives is imperative in creating a pathway to financial sustainability. Historically, many hospital boards have started their financial planning with the assumption that volume will increase year over year, and in turn, avoid tough decisions about where to cut costs.
But succeeding in a more challenging financial environment requires a more disciplined, data-oriented approach that reflects previous performance, blends financial and clinical analytics, and begins with a clear understanding of how far the organization will need to go to create a sustainable path forward.
Exhibit 1: Overall Medicare margin dropped slightly from 2016 to 2017
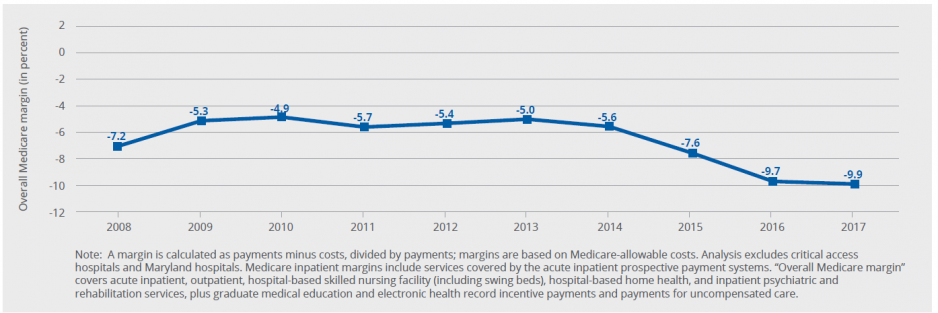
Source: 2019 MedPAC analysis of MedicAre cost reports from CMS
While each organization will need to develop and refine its target by assessing a range of clinical, financial, and market-specific factors, establishing an initial goal of breaking even on Medicare payment can be an effective minimum benchmark at the outset—and one that requires most hospitals to dramatically improve their performance.
According to the Medicare Payment Advisory Commission, the average Medicare margin for hospitals was -9.9 percent in 2017; even hospitals providing high-quality care at lower costs performed at -2 percent. However, according to the Kaufman Hall/HFMA 2019 Healthcare Performance Improvement survey, 84 percent of respondents said their organizations’ target for cost reductions over the next three years was 10 percent or less.
Emerging systems allow organizations to integrate data on financial and clinical performance, and analyze indicators ranging from productivity to service utilization to cost-effectiveness. Current comparative analytics tools also allow hospitals to access real-time or predictive data, a major improvement from traditional retrospective data.
Increased data on its own, however, will not necessarily lead to improvements in performance. Hospitals run the risk of becoming data rich and information poor, with harried department leaders deluged with monthly analytics reports that are more a source of noise than actionable information.
Comparative analytics systems that compile and provide benchmarks for similar institutions can help hospital leaders better understand how their performance aligns with and varies from peers. These efforts should be grounded in developing a meaningful understanding of why variance from benchmarks occur before potential adjustments are determined.
For instance, an organization might discover that it’s staffing an additional clinical full-time employee (FTE) in a different service line than its peers. However, the FTE in question might be staffed to address a specific clinical need – and could have an outsized impact on patient care or satisfaction.
Establishing a results management office
Organizations can only make the most of their analytics when their leaders and staffs are empowered to act on the analytics’ findings. Many organizations have created specific performance improvement champion roles, with the intent of empowering a senior leader to drive change and take accountability for organization-wide results. However, this approach can sometimes hamper accountability at the department or individual unit level by creating the perception that the champion is solely responsible for the success or failure of the project.
A results management office that reports and tracks results—but is not responsible for the performance of individual departments—offers an approach to accountability throughout the entire enterprise.
One hospital in a mid-sized Midwest city, facing a $15 million performance gap projected to grow to $40 million in five years, performed a comprehensive assessment to identify areas of improvement across the entire enterprise. As part of its overall cost reduction effort, the system established a results management office charged with answering the following questions:
- What are the services we are using?
- Are we using them in an optimal way?
- How can we maximize the effectiveness of our spending to provide the level of service and product that are important to both patients and clinicians?
The office reported results to the system’s controller, who reported directly to the chief financial officer. The results management office, in its role monitoring organizational change, also offered project management assistance to those responsible for specific initiatives. Two years into the initiative, the system hit 96 percent of its overall cost management target.
Pitfalls
- Making budgeting determinations based on the assumption that volume will increase
- Narrow focus on peer group performance
- Flooding staff with too much data
Best Practices
- Analyzing prior performance as a predictor of future volumes
- Probing into the root causes of variance
- Training staff to effectively use real-time data
An Integrated Approach to Reducing Clinical Variation
For all hospitals, clinical variation is a persistent and institution-wide challenge, leading to both higher costs and more uneven performance on the quality of care delivered. According to the cost transformation survey, 25 percent of respondents cited unwarranted clinical variation as the area where their organization faced the most difficulty achieving its cost transformation goals.
Exhibit 2: Cost Management Is a Continuous Process

All too often, though, traditional hospital performance improvement projects are limited to narrowly focused projects like reducing healthcare-acquired infections or sepsis. But a more holistic approach is emerging, which examines data for case management, care variation, and length of stay collectively have an opportunity to truly address full episodes of care.
Physician engagement in efforts to reduce clinical variation is also critical and requires data that blends information on cost and quality metrics. Only 14 percent of respondents to the cost transformation survey said their clinicians would agree they had access to actionable information to address unwarranted clinical variation.
Ideally, data sets should cascade down from a physician group to individual service lines, physicians, and patients, and include severity and risk adjustments. As scientists, physicians tend to be skeptical of data – and might make arguments about the severity of their patients. Severity-adjusted cost by case data is a way of addressing those concerns.
Software systems should also stay current, incorporating current rules and guidelines from the Centers for Medicare & Medicaid Services and the Centers for Disease Control and Prevention to keep physicians informed.
Upcoming articles in this series will take a deeper look at reducing clinical variation and engaging physicians in cost transformation.
Pitfalls
- Implementing one-off improvement projects
- Failing to address physician concerns about the impact on quality
Best Practices
- Focusing improvements on the full episode of care
- Using severity-adjusted data
A New Era of ‘Workforce Optimization’
Whether it’s delivering millions of packages on time to customers’ doorsteps, managing thousands of flights in multiple time zones, or deploying military personnel across the globe, organizations in numerous industries tap into the power of logistics science and optimization modeling every day.
But for hospitals and health systems, the challenge of getting the right nurse to the right tower for the next shift without exceeding the staffing budget or upsetting the nurse-to-patient ratio is perennially frustrating.
As workforces evolve, the traditional approach of using the midnight census as the chief measure of patient demand can obscure more granular trends measured in hours or minutes. Without access to accurate, timely data, hospitals run the risk of over-staffing, and the prospect of tens of millions of dollars in increased costs. At the other end of the spectrum, under-staffing can jeopardize clinical quality, staff engagement, and patient satisfaction.
Emerging workforce optimization modeling can help organizations review years of staffing and budgeting information on data points ranging from hourly patient demand to clinical time entry, to bed capacity to nurse-to-patient ratios. The process is intended to uncover potential inefficiencies and changes in operation that might require modifications in work rules or scheduling protocols.
For workforce optimization, data can dispel myths. For instance, many organizations might still cling to the idea that nurses are averse to working in float pools. But those assumptions can often be based on the preferences of Baby Boomers – and not the Millennial and Generation Z employees making up a bigger share of the population.
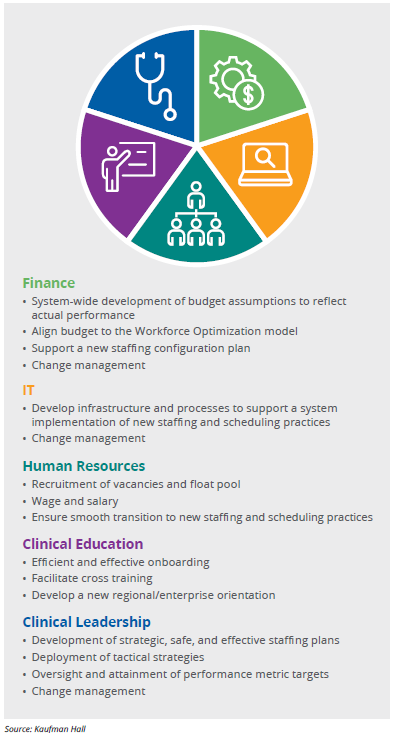
Achieving meaningful results of that nature requires genuine buy-in and engagement from multiple internal stakeholders, including the chief nursing officer, the chief finance officer, human resources leaders, schedulers, and frontline nursing staff. Initial meetings might help each department understand how their counterparts traditionally perceive and measure staffing, and can also help ensure appropriate staffing levels have been met.
For example, while members of the finance department might view staffing through the lens of a given number of FTEs in a unit, frontline staff are more likely to focus on the number of patients they see in a given day. And the chief nursing officer often ends up mediating between both groups.
When optimization efforts are inclusive of a wide range of viewpoints and needs, they can deliver results that satisfy multiple internal stakeholders. Finance leaders might appreciate greater alignment between projecting staffing budgets and actual results, while frontline nurses may enjoy greater predictability in the day- to-day staffing of their particular unit. Ideally, workforce optimization can help organizations adapt and thrive in an ever-shifting environment, and achieve results ranging from improved financial performance to a more engaged clinical staff.
Pitfalls
- Using the midnight census to determine demand
- Falling back on long-held beliefs about staff work preferences
- Allowing siloed departments to view results too granularly
Best Practices
- Optimizing scheduling with more timely data
- Adjusting staffing approach to reflect preferences of Millennials and Generation Z
- Team-based approach engaging nursing, finance, and human resources
Exhibit 3: A Multidisciplinary Approach to Workforce Optimization
Managing the Supply Chain
Hospitals and health systems count on their supply chain to manage what can account for as much as 40 percent of an organization’s costs. As increasing attention focuses on patient outcomes and experiences, the supply chain must establish processes that enable tracking of purchased products and services through to individual patient encounters. Cost containment within existing operations is an imperative not only to maintain margins within a tightening payment environment, but also to free up the resources needed to invest in new care models and technologies.
Supply chain leaders need to benchmark their performance, both internally and against peer organizations, for two reasons. First, a comparative framework enables supply chain leaders to identify opportunities for improvement in areas where their performance is lagging behind that of their peers or not moving in the right direction. Second, a combination of internal and external benchmarks can demonstrate to the supply chain and the clients it serves how consistently it is performing within the organization and how well it is performing against peer organizations. Where the supply chain excels, a comparative analytics framework can validate and quantify the supply chain’s contributions to the organization.
Cost and utilization data enable supply chain leaders to detect variations across departments and facilities, and identify areas where product standardization could generate savings, support bundled-payment and pricing initiatives, or provide greater leverage for volume-based discounts from vendors. Utilization data can support predictive modeling for demand trends that supply chain managers can use to ensure sufficient inventory is on hand.
For many organizations, providing this data at the needed level of granularity and timeliness will require investment in more sophisticated cost accounting, inventory management, and clinical systems. The benefits of this investment will extend beyond the supply chain, however, to include both finance and the organization’s clinical enterprise.
The Future of Cost Reduction: Making Tough Decisions About Existing Facilities
The future environment for hospitals and health systems remains uncertain. Well-financed technology companies and retailers press forward with new, consumer-friendly care models, while public and private payers and employers put increasing pressure on hospitals to control costs and maximize quality.
To sustain operations in the new environment, hospitals and health systems must press forward with comprehensive, integrated cost reduction efforts that set realistic targets, truly engage all facets of operations, and are designed for long-term continuous improvement.
But simply focusing on clinical variation, workforce optimization, and supply chain improvements is no longer enough to support the investments needed to take on new competitors and adjust to increasing payment pressures.
Hospital and health system leaders must also take on the difficult challenge of assessing whether their facilities are still providing value – or whether the changing environment necessitates possible facility closures. According to a 2018 study by the American Hospital Directory, there are 13 states in which average hospital occupancy rates for urban hospitals were 50 to 60 percent, and 28 states in which average occupancy rates for rural hospitals were 40 percent or less. These averages mask even greater variation from facility to facility within smaller areas.
While traditional cost-reduction efforts remain vital, the ability to make tough decisions about facilities that are no longer creating necessary healthcare value is essential to maintaining relevance in a competitive and rapidly shifting industry.









