
For nearly all health systems, oncology services are an important driver of financial stability and growth. And as cancer care increasingly embraces precision medicine and personalized therapies, health systems must evolve accordingly.
Partnerships between health systems and National Cancer Institute (NCI) centers, for example, hold the promise of leveraging the specialized expertise of academic centers with the broader patient populations of health systems—all with the end goal of providing state-of-the-art oncology care close to home. These partnerships have several important benefits:
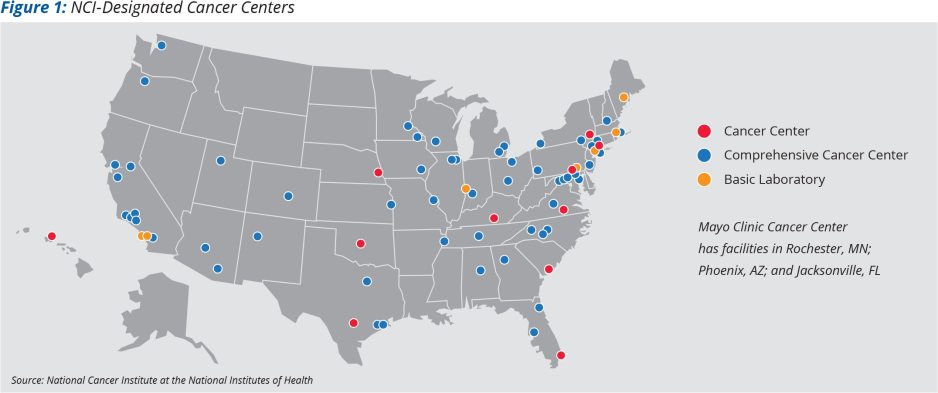
- Expanding access to cancer care for entire populations. Many states in the United States (Figure 1) have no NCI center, underscoring the need to leverage the reach of local health systems.
- Ensuring access to quality care and advanced treatments is an important goal for health systems seeking partnerships with NCI centers. Interest in precision oncology—an evolving approach to cancer care that considers individual variability in the genes, environment, and lifestyle of each patient—is accelerating rapidly, and health systems and NCI centers alike are racing to develop related capabilities.
- Advancing research goals is another key benefit of partnerships for NCI centers on topics ranging from vaccine development to genetic treatments to targeted precision therapy. Partnerships with local health systems can deliver the expanded and diverse patient populations needed for successful clinical trials that spur accelerated innovations on precision oncology and other areas. For patient populations, access to clinical trials and education about their value is especially important.
Developing partnerships with appropriate structures and common goals is critical, given the myriad forms and variable degrees of benefits among existing partnership models. In fact, most cancer partnerships today are brand-oriented, research or clinical affiliations that do not drive economic and clinical integration, and therefore do not create a meaningfully differentiated platform for mutual growth and advancement. Moving toward more truly integrated clinical and economic structures provides opportunities for shared growth that position partners for success in the oncology market moving forward. Key partnership goals may include:
- Creating the type of joint clinical model required for advancing quality outcomes (e.g., an integrated multidisciplinary approach to oncology care) and achieving volume growth for each party (e.g., coordinated care transitions for the highest-acuity patients)
- Creating a seamless patient experience that drives consumer preference for the partnership’s services
- Creating a balanced economic model that incentivizes the joint pursuit of growth initiatives and the required dedication of time investment required for a self-sustaining partnership
- Aligning missions and creating shared core values that build a foundation of trust and a common approach to executing the partnership’s work
A Kaufman Hall analysis discovered that most partnerships can be described as research or clinical/branding affiliations (Figure 2).
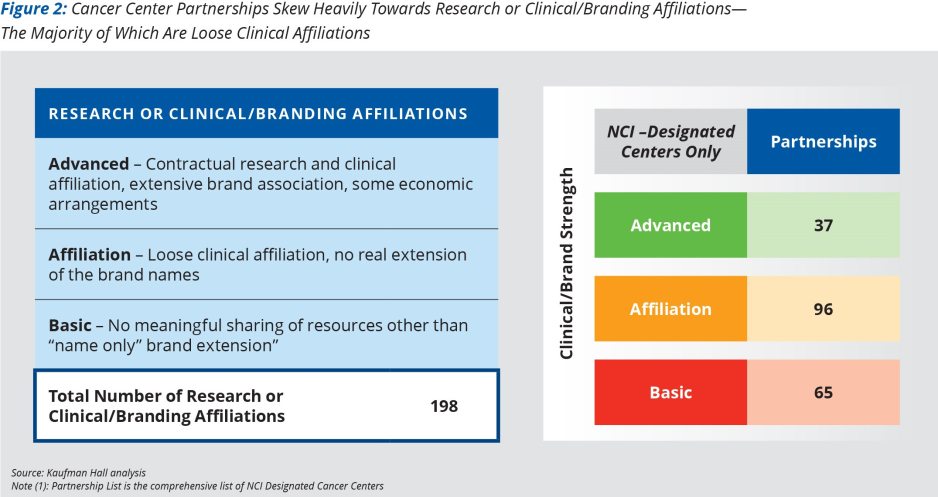
Out of at least 198 clinical/branding partnership arrangements identified, organizations further fell into three subcategories:
- Advanced - Contractual research and clinical affiliation, extensive brand association, some economic arrangements (19% of all such partnerships)
- Affiliation - Loose clinical affiliation, no real extension of brand names (48%)
- Basic - No meaningful sharing of resources or brand, other than a name-sharing system (33%)
Conclusion: How to build a beneficial partnership
Oncology partnerships are not the answer in every market. Indeed, partnerships are nuanced and complex, and require consideration of the appropriate structuring considerations as there is no one-size-fits-all model. Absent a rigorous approach to standing up the optimal partnership, the failure rate is high, with several possible pitfalls:
- Organizations should avoid “in name only” brand extension arrangements without clear clinical benefits to patients. Creating true economic and clinical integration often creates a more sustainable model characterized by shared incentives.
- Partnerships which do not meaningfully improve access to leading cancer care for patients in community system markets are not likely to succeed.
- Partners that do not consider how cancer care is evolving or thoughtfully consider the competitive and community response to the partnership are also unsuited for long term success.
There are many factors to consider given the potential complexity of oncology partnerships, and a well-structured partnership process can help parties get to a meaningful and mutually beneficial arrangement. Key principles of a successful partnership process include:
- Establishing a shared vision, common goals, and mutually beneficial incentives that encourage resource allocation to sustain to the partnership
- Initiating a dedicated oversight (e.g., governance, management) structure to support the clinical, operational, and strategic goals of the partnership
- Developing a rubric to assess the partnership’s ability to serve community needs for oncology care
- Developing a strategic viewpoint and tactical steps to take, depending on what cohort the partnership is designated as in the assessment
- Developing strategic and economic scenarios that may impact that cohort, and planning accordingly
- Engaging physicians in the development of the partnership at an early stage in the process
- Structuring the economic and clinical elements of the partnership for sustainability over the long-term
- Taking steps to creating a combined culture that can adapt to a rapidly changing environment
- Laying the groundwork for real-time data-sharing to support both patient outcomes and research integration into clinical care











